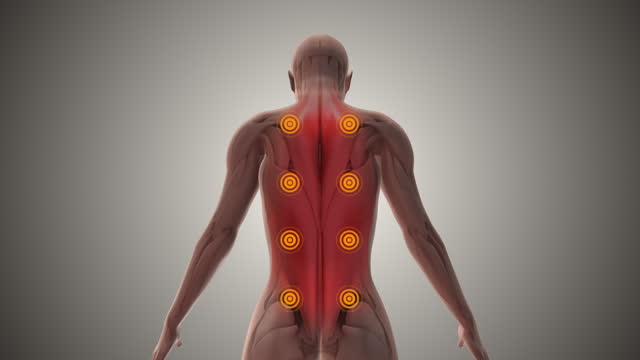
Trigger points (TrP) are hyperirritable spots, palpable nodules in the taut bands of the skeletal muscle fascia. Direct compression or muscle contraction can elicit a jump sign, local tenderness, and local twitch response.
response and referred pain which usually responds with a pain pattern distant from the spot.
Jump Sign:
Jump sign is the characteristic behavioural response to pressure on a TrP. Individuals are frequently startled by the intense pain. A jump sign thus reflects the extreme tenderness of a TrP. This sign has been considered pathognomonic for the presence of TrPs.
Local Twitch Response:
It is defined as a transient visible or palpable contraction of the muscle and skin as the tense muscle fibers contract when pressure is applied through needle penetration or by snapping palpation.A local twitch response on stimulating active TrPs is a widely accepted diagnostic sign.
Referred pain:
It is also called reflective pain, is pain perceived at a location other than the site of the painful stimulus. Pain is reproducible and does not follow dermatomes, myotomes, or nerve roots. There is no specific joint swelling or neurological deficits. Pain from a myofascial TrP is a distinct, discrete and on constant pattern.
Anatomy:
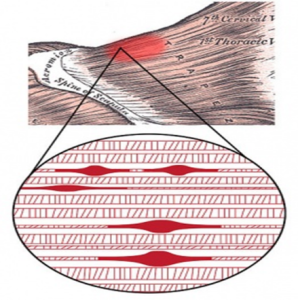
Trigger points develop in the myofascia, mainly in the centre of a muscle belly where the motor endplate enters. Those are palpable nodules within the tight muscle at the size of 2-10 mm and can be demonstrated at different places in any skeletal muscles of the body. We all have TrPs in the body. When it happens, TrPs are directly associated with myofascial pain syndrome, somatic dysfunction,
psychological disturbance and restricted daily functioning.
Causes:
- Ageing,
- Lack of exercise – commonly in sedentary life style.
- Bad posture.
- Muscle overuse and respective micro-trauma – weightlifting.
- Chronic stress condition.
- Anxiety, depression, psychological stress trauma.
- Sleep disturbance.
- Joint problems and hypermobility.
Trigger points can significantly impact conditions like Quadratus Lumborum Syndrome. These localized areas of muscle tightness can cause severe pain and affect the stability and movement of the lumbar spine.
Classification of TrPs:
Primary or Central TrPs are those that cause severe pain locally at the pressure with irradiation according to the referred pain. Usually are based around the center of a muscle belly.
Secondary or Satellite TrPs arise in response to existing central trigger points in surrounding muscles. Can be present in the form of a cluster.
Active TrP is any point that causes tenderness and referred pain on palpation. Palpation may also cause autonomic symptoms such as skin redness, sweating, and dizziness.
Inactive and latent TrP does not evoke pain spontaneously, and local or referred pain occurs only with strong digital pressure.
Diffuse Trigger Points Commonly happens in case of severe postural deformity where initially primary TrPs are multiple, so secondary multiple TrPs are only a response of a mechanism, called diffuse.
Attachment Trigger Points Arise in tendo-osseous junctions which become very tender. If not treated, degenerative processes of an adjacent joint can spring up.
Ligamentous Trigger Points Even ligaments can develop trigger points. The presence of TrPs in the anterior longitudinal ligament of the spine can result in neck instability.
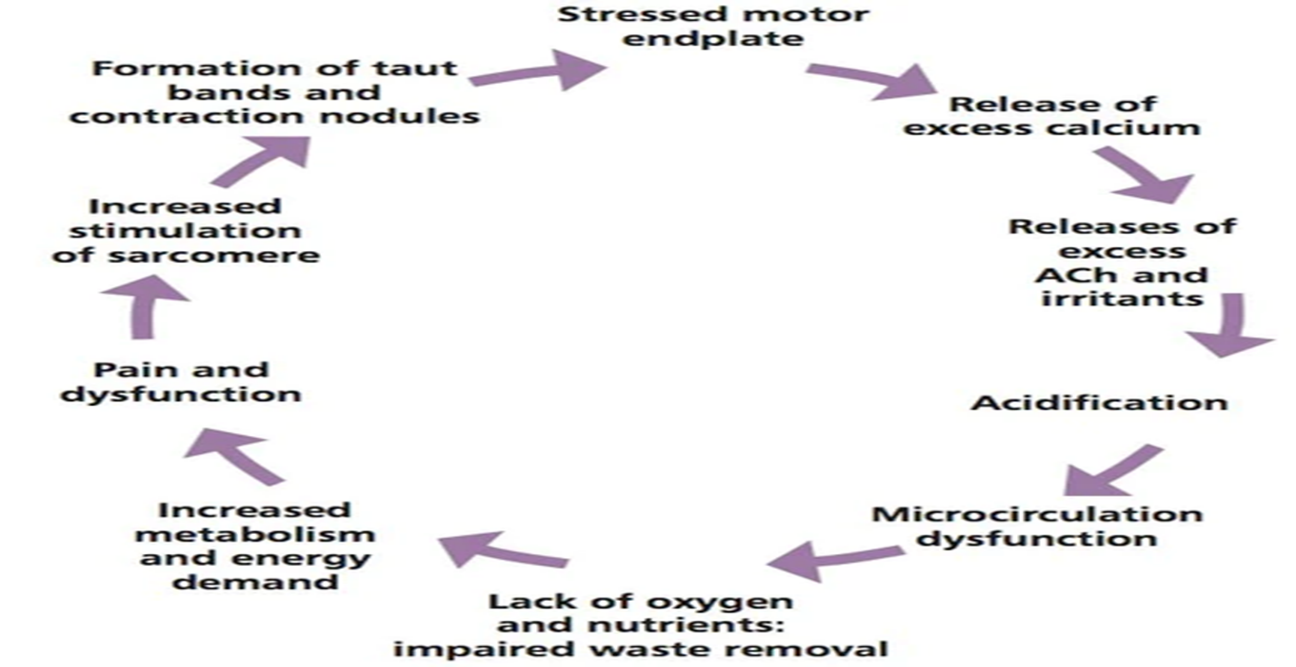
Pathogenesis:
There are some theories written in literature that try to explain the formation, sensitization, and manifestation of TrPs, but few of them have strong evidence. Under normal conditions, pain from TrPs is mediated by thin myelinated (A-delta) fibres and unmyelinated (C) fibres. Various noxious events, such as mechanical stimuli or chemical mediators, may excite and sensitize Ad fibres and C fibres and thereby play a role in the development of TrPs.
Theories:
Integrated Trigger Point Hypothesis (ITPH):
It is the present working hypothesis. When sarcomeres and motor endplate become overactive for a number of different reasons, pathological changes start at cellular levels. This turns on permanently sarcomeres leading to a local inflammatory response, loss of oxygen supply, loss of nutrient supply, endogenous (involuntary) shortening of muscle fibres, and increased metabolic demand on local tissues.
Trigger point manifest in the region where sarcomeres and motor endplates become overactive.
Polymodal theory:
It explains the existence of polymodal receptors (PMRs) throughout the body which under certain constant, pathological stimuli turn into trigger points.
Radiculopathic theory:
It explains the direct relationship between problems on nerve roots which lead to local and distant neurovascular signals and trigger points creation.
Differential Diagnosis:
Musculoskeletal Diseases
- Occupational myalgias
- Post-traumatic hyperirritability syndrome
- Joint dysfunction (osteoarthritis)
- Tendonitis and bursitis
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.