Bertolotti syndrome, named after the Italian physician Mario Bertolotti who first described it in 1917, arises from a congenital anomaly known as lumbosacral transitional vertebrae (LSTV). This condition, often overlooked, can lead to significant back pain, typically emerging in one’s late twenties to early thirties, though occasional instances manifest earlier.
The syndrome involves an anatomical variation where the lowest lumbar vertebra (L5) exhibits abnormalities in its connection to the sacrum or ilium. This can include fusion or an abnormal pseudoarticulation, altering the biomechanics of the spine.
Bertolotti Syndrome Clinical Presentation:
Bertolotti Syndrome presents with chronic and persistent lower back pain, often accompanied by buttock pain and radicular symptoms that radiate along the nerves into the legs. It is characterized by the presence of a transitional vertebra, which can sometimes be mistaken for or coexist with other lumbar spine conditions like PLID (Prolapsed Lumbar Intervertebral Disc).
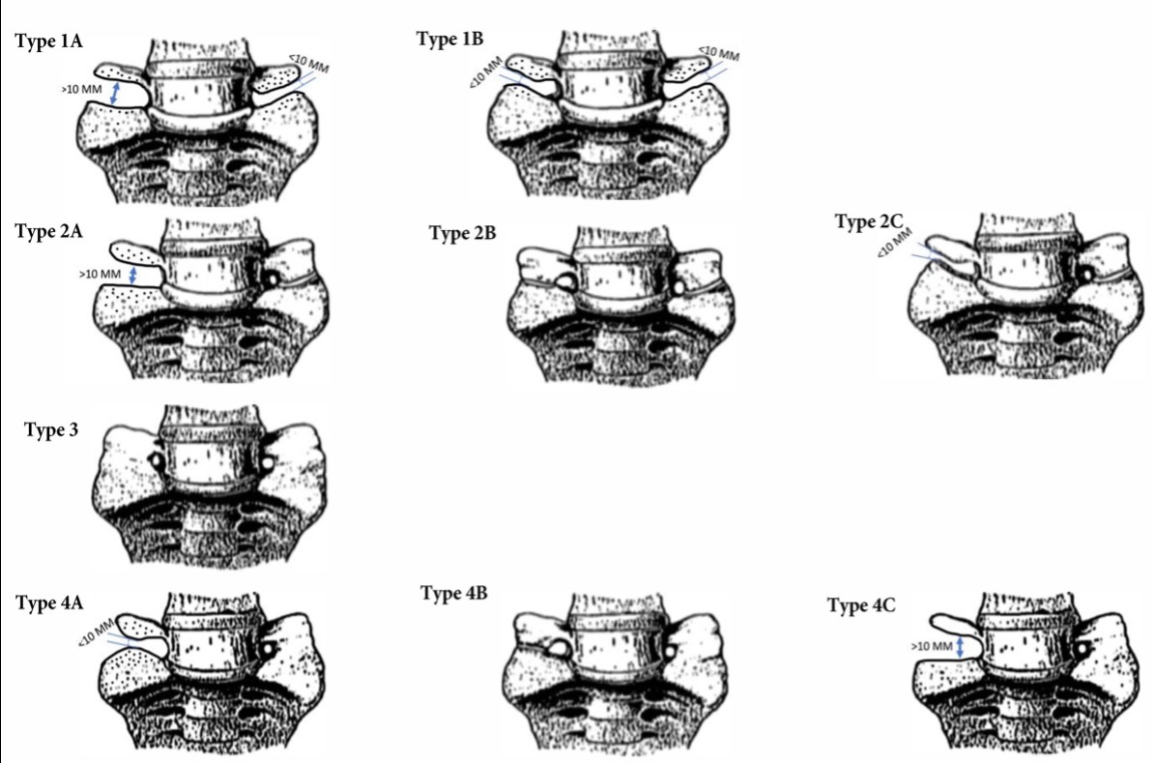
Classification:
Bertolotti Syndrome is classified according to the Jenkins Classification, which categorizes the anatomical variations observed in the lumbosacral transitional vertebrae (LSTV). The classification system includes four main types:
Type 1: This type features a dysplastic transverse process at the L5 vertebra with a gap that ranges from more than 2mm to less than 10mm across the lumbosacral junction.
Type 2: In Type 2, there is a pseudo-articulation between the transverse processes of the L5 vertebra and the sacrum or ilium, where the gap is less than 2mm.
Type 3: Type 3 involves complete fusion of the transverse process with the sacrum or ilium, occurring lateral to the facet joint at the ala. There is no spontaneous fusion of the disk or facet joints in this type.
Type 4: Type 4 is characterized by unilateral fusion on one side (Type 4A), bilateral fusion (Type 4B), or a combination of Type 2 anatomy on one side with Type 3 on the contralateral side (Type h4C). Additionally, Type 4 variants may involve contact with the iliac bone on either the left (+L) or right (+R) side.
Epidemiology:
The reported incidence of Bertolotti syndrome ranges from 4% to 8% within the general population, whereas the occurrence of lumbosacral transitional vertebrae (LSTV) is more prevalent, estimated between 4% to 30%. This disparity suggests that Bertolotti syndrome may be significantly underdiagnosed by healthcare providers.
Furthermore, among individuals with LSTV, those experiencing associated pain are more commonly male than female, with the prevalence of pain-related LSTV being more than twice as high in males compared to females.
Treatment:
Treatment options include nonsteroidal anti-inflammatory drugs (NSAIDs), physical therapy, injections, radiofrequency ablation, and surgery.
Physical therapy treatment:
- Core strengthening Exercises
- Stretching Exercises
- Lumbosacral region Mobilization Techniques
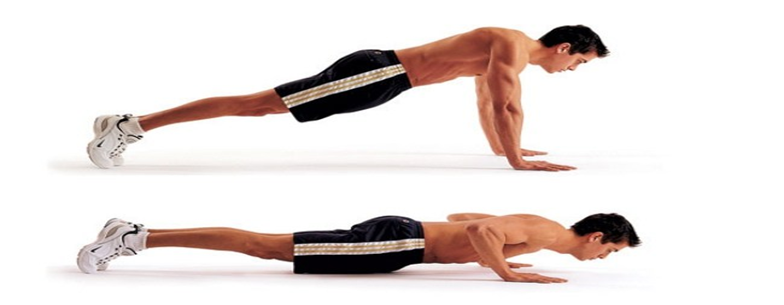
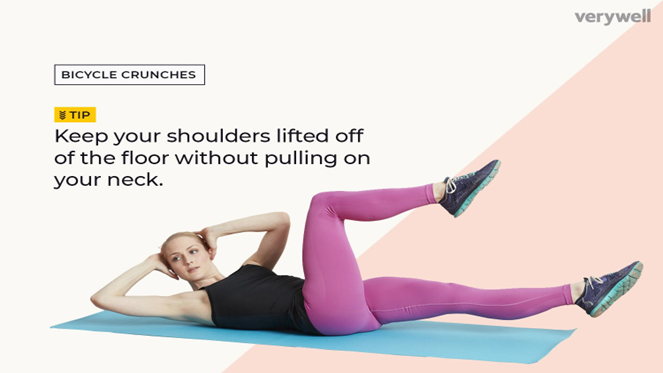
Core Strengthening Exercises:
Bridging

Leg Raise

Bird Dog

Push Ups
Bicycle Crunch
Crunches

Lumbosacral Mobilization Technique:
Posteroanterior (PA) mobilizations of the lumbar spine are achieved by applying a force on to a vertebral segment in a posteroanterior direction (Back to front). PA mobilizations are a commonly used manual therapy technique that has shown to be effective at reducing pain in patients with low back pain (LBP).
Procedure:
Starting Position:
Patient lying in prone. Therapist stands to side of patient placing their ulnar surface of hand over the selected spinous process (SP) with their wrist in full extention. Other hand placed ontop of hand to reinforce. Therapist’s shoulders should be directly above with elbows slightly bent.
Method:
Therapist uses their body weight to apply a PA force to the selected SP by leaning their body over their arms and performing rocking movements to provide oscillatory movements of the vertebra.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.