Coccygodynia, also known as coccydynia or coccalgia, refers to the experience of pain localized in the coccyx region. Typically, this pain is exacerbated when sitting or transitioning from sitting to standing. While many cases resolve within several weeks to months, some individuals may develop chronic pain that significantly affects their quality of life.
Epidemiology and Etiology:
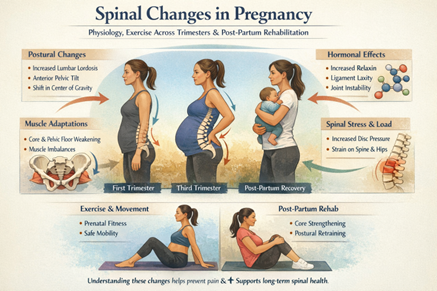
The incidence of coccygodynia is currently not well-documented. Several factors increase the risk of developing coccygodynia, including body weight, age, and gender. Obesity can elevate intrapelvic pressure during sitting, potentially causing the coccyx to displace backward (posterior subluxation). Conversely, rapid weight loss can deplete cushioning around the coccyx, leading to forward displacement (anterior subluxation). Females face a significantly higher risk, potentially due to increased pelvic pressure during pregnancy and childbirth. Coccygodynia is more prevalent in adults and adolescents compared to children.
Coccygodynia is categorized as post-traumatic, non-traumatic, or idiopathic. Post-traumatic cases often stem from external trauma like falls or childbirth-related injuries, as well as repetitive strain from prolonged sitting on hard surfaces. Non-traumatic causes may involve degenerative disc disease, sacrococcygeal joint mobility issues, infections, or anatomical variations in coccyx configuration, particularly types II, III, and IV. Idiopathic coccygodynia refers to cases where no specific pathology is identified, often diagnosed by excluding other conditions. Muscular abnormalities like levator ani muscle spasticity can also contribute to coccyx misalignment in some cases.
Clinical Presentation:
- The primary symptom of coccygodynia is localized pain in and around the coccyx, typically without severe low back pain or radiating symptoms
- The pain is commonly centered on the sacrococcygeal joint and is often described as a “pulling” or “cutting” sensation.
- Patients frequently experience tenderness when the coccyx is palpated.
- Individuals with coccygodynia often adopt a protective seated posture, where they elevate one buttock to reduce pressure on the coccyx.
- Pain tends to worsen with prolonged sitting or when transitioning from sitting to standing.
- Relief is often found by sitting on the legs or one buttock.
- Additional symptoms may include pain during defecation or an increased urge to defecate.
- Some patients report exacerbation of pain during activities like coughing or menstruation in females.
Management:
Conservative or non-surgical approaches are generally preferred for treating coccygodynia and are successful in approximately 90% of cases. These treatments typically involve non-steroidal anti-inflammatory drugs (NSAIDs) for pain relief, along with activity modifications, ergonomic adjustments, and physical therapy to alleviate symptoms and improve function.
Surgical intervention, such as coccygectomy (partial or complete removal of the coccyx), is considered only when conservative treatments fail to provide relief from coccygeal pain. Coccygectomy is the most common surgical procedure performed for severe cases of coccygodynia.
Similar to coccydynia, or tailbone pain, ischial bursitis is also a condition that can cause discomfort in the lower back and pelvic region. Ischial bursitis involves inflammation of the bursa near the ischial tuberosity, while coccydynia refers specifically to pain in the tailbone area. Proper diagnosis and treatment for these conditions are essential for managing symptoms and improving quality of life.
Physical Therapy Management:
Ergonomic Adjustments:
The primary aim of treatment initially focuses on educating individuals about proper posture. Physiotherapists often recommend the use of cushions to alleviate coccygeal pressure while sitting. Wedge-shaped coccygeal cushions, available over-the-counter, are designed to reduce coccyx pressure. Alternatively, donut-shaped or circular cushions may also be used, although donut-shaped cushions can sometimes increase pressure on the coccyx but are beneficial for relieving rectal pain. The use of cushions is typically recommended for a period of 6-8 weeks.
Manual Therapy:
Manual therapy techniques recommended in the literature encompass a variety of approaches, including both internal and external methods targeted at alleviating coccygeal pain.
Internal techniques may involve massaging the levator ani or coccygeus muscles, mobilizing the coccyx while hyperextending to stretch the levator ani muscle, or performing repeated mobilizations with coccyx rotation.
External techniques may include manipulating the coccyx or sacroiliac joint, mobilizing the sacrococcygeal or intercoccygeal joints, performing posterior mobilizations to the thoracic spine, and stretching the piriformis or iliopsoas muscles.
Including thoracic spine mobilizations can address compensatory patterns affecting the entire spine and pelvis, potentially influencing coccygeal pain. Similarly, mobilizations focusing on the lumbar spine can impact pelvic tilt and alignment, which directly affects the position and stress on the coccyx. These approaches aim to provide relief and improve function without surgical intervention.
Physical Therapy Modalities:
In a study by Lin et al. (2015), it was found that extracorporeal shockwave therapy (ESWT) was more effective than shortwave diathermy and interferential current (IFC) in reducing pain scores measured by the visual analogue scale. Patients treated with ESWT reported higher subjective satisfaction scores.
The mechanism behind ESWT’s effectiveness in coccygodynia is still under debate in the literature. However, it is suggested that ESWT may decrease the inflammatory response and expression of inflammatory mediators associated with coccygodynia by inducing neovascularization.
Comparatively, Lin et al. (2015) noted that while IFC and shortwave diathermy also reduced pain scores, their efficacy did not match that of ESWT. In contrast, a study by Wray et al. (1991) reported minimal benefits from a combination of ultrasound and shortwave diathermy treatments, with only 16% of patients experiencing symptom relief after 2 weeks of each therapy.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.