Ischial bursitis, also known as Ischiogluteal bursitis, Weaver’s bottom, or Tailor’s bottom is a rare and infrequently recognized bursitis of the buttock region. It’s one of the four types of hip bursitis. The bursitis is mainly due to chronic and continuous irritation of the bursa and occurs most often in individuals who have a sedentary life. The irritation commonly results from prolonged pressure on the ischium, Bursitis always develops in response to another pathology. Ischial bursitis can result from sitting for long periods on a hard surface, from direct trauma to the area, or from injury to the hamstring muscle or tendon through activities such as running or bicycling.
Anatomy:
The Ischial bursa is a deep-located bursa over the bony prominence of the Ischium and lies between the Gluteus Maximus and the Ischial tuberosity.
Etiology:
- Trauma (hemorrhagic bursitis).
- Inflammation (rheumatoid arthritis and spondyloarthropathies).
- Infection (rarely septicemia and septic arthritis ).
- Crystal deposition. There are three basic crystal-induced arthropathies: monosodium urate crystal deposition disease(gout); calcium pyrophosphate dihydrate (CPPD) crystal deposition disease (pseudogout and other clinical presentation); and calcium hydroxy-apatite (HA) crystal deposition disease.
- Cycling, because it involves a lot of gluteus maximus muscle repetition.
Pathophysiology:
There are several different types of bursa, including synovial, subcutaneous, submuscular, and adventitious. The ischial bursa is synovial, which means it is made up of a capsule of fatty connective tissue and synovial fluid. The cells of the synovia multiply in response to infection or irritation, increasing the amount of synovial fluid produced. This process is mediated by inflammatory mediators like cytokines, cyclooxygenase, and metalloproteases. The end outcome is a thick cavity filled with fluid and abundant fibrin, resulting in the creation of granulation tissue. This granulation tissue will end up altering the normal activities of other surrounding tissues, like the muscles, tendons, or bones.
Clinical Presentation:
- Pain in the region of the ischial tuberosity which may also be referred to the lower leg.
- Pain is aggravated by prolonged sitting.
- Pain with passive hip flexion.
- Pain with stretching, which also causes an inability to extend the hip.
- Tenderness may occur over the ischial tuberosity.
- Inability to sleep on the affected hip.
- Regional muscle dysfunction.
- Swelling and limited mobility.
- Overlying erythema. If erythema forms the major part of the presentation, etiologies such as cellulitis or septic joint are suspected.
Differential Diagnosis:
Ischial Bursitis can be confused with myxoid tumors. These are a group of rare tumors showing myxoid change, including neurofibroma, schwannoma, and myxoma. Therefore it may be necessary to do an incisional or excisional biopsy. By using this technique the doctors take cells out of the injured place and they can histologically differentiate cells from a myoxoid tumor or Ischial Bursitis. An X-ray also rules out the possibility of a stress fracture or roughening of the cartilage in the hip joint.
Examination:
- Pain with a straight leg raise test is often present.
- Actively resisted extension of the affected hip reproduces the pain.
- Plain radiographs may reveal calcification of the bursa and associated structures which is consistent with chronic inflammation.
- Examination of patients with ischial bursitis reveals a soft tissue mass in the gluteal region of the affected hip. This soft tissue mass is described as well-defined, non-mobile, and slightly tender.
Ischial bursitis and coccydynia or tailbone pain are both conditions that can cause discomfort in the lower back and pelvic region. Ischial bursitis involves inflammation of the bursa near the ischial tuberosity, while coccydynia refers to pain in the tailbone area. Proper diagnosis and treatment for these conditions are essential for managing symptoms and improving quality of life.
Physical Therapy Management:
Rest: The treatment begins with rest. Rest in the meaning of keep on doing your daily activities and sports but at a lower intensity.
Cold therapy: Cold therapy contains ice application with cold packs usually for about 20-30 minutes.
Ultrasound therapy, transcutaneous electrical stimulation and laser can be used for improving the healing process and reducing pain.
Heat treatment is also possible, with hot packs. It increases blood flow and oxygen tension.
Frictional Massage: It is recommended to use friction massage in addition to the therapy on chronic bursitis because it affects the adhesions in chronic bursal problems. It breaks down scar tissue, increases the extensibility and mobility of the structure, promotes normal orientation of collagen fibers, increases blood flow, reduces stress levels, and allows healing to take place. Friction massage is beneficial to the underlying structures. The Graston technique is most commonly used in frictional massage.
Graston Technique: The Graston Technique is a manual therapy that uses stainless steel instruments to perform muscle mobilization. The tools are used in two ways: Practitioners move the instruments over the skin to find any muscle knots, fibrous tissue, or scar tissue that can cause the patient pain or restrict movement.
Protocol: The seven-part protocol includes: an exam, warm-up, treatment (30-60 seconds/treatment), post-treatment stretching and strengthening, and ice. The Graston instruments are either concave or convex in shape. The practitioner uses the concave shape to apply pressure over a large area, promoting comfort during treatment.
Therapeutic exercises:
It should contain stretching exercises to increase the flexibility of the tight hamstring muscle and reduce pressure on the bursa and achieve painless motion and strengthening exercises, to correct muscle imbalances, ease symptoms. Static stretching is believed to be the safest method because it would have the lowest injury risk. It is most effective when you stretch once a day, 30 seconds for each stretch. The benefits of static stretching include preventing the tissue from absorbing great amounts of energy per unit of time, not eliciting a forceful reflex contraction and it is good against muscle soreness.
Examples of static stretching exercises:
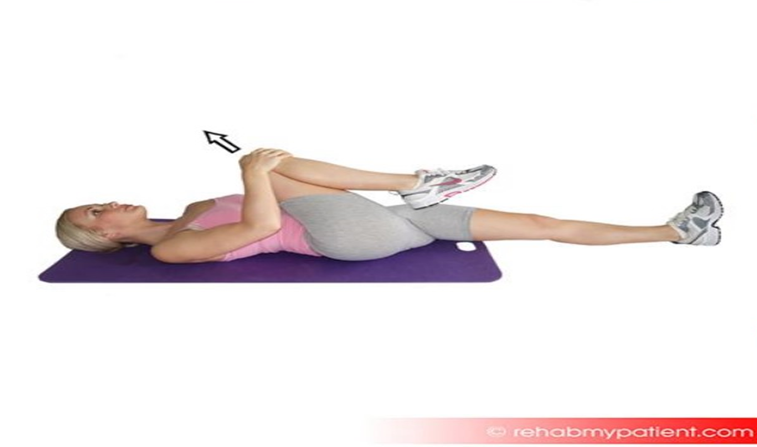
Gluteus stretch: Lie on your back and bend your affected knee upward. Grab the back of your knee with both hands and slowly pull the knee toward your chest. Hold this position for 5 to 10 seconds and repeat 6 to 10 times.
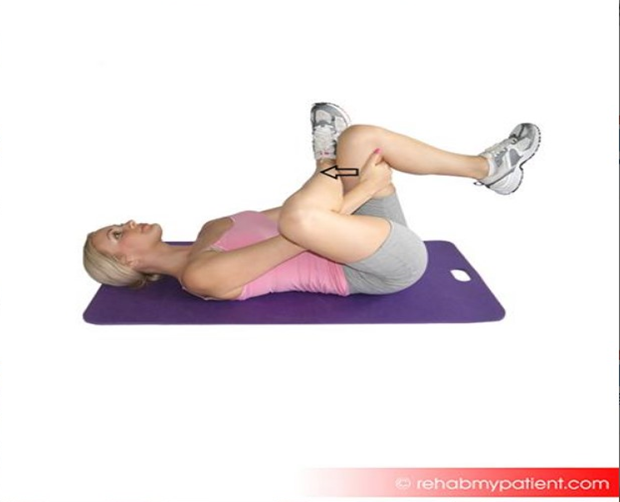
Piriformis stretch: While lying on the floor, bend your affected knee and cross the leg over the other leg, placing your foot alongside the knee. Use your hands to pull the good leg in towards you, lifting the leg off the floor. You should feel a stretch in the affected buttock and in your outer thigh. Hold this position for 10-30 seconds.
Strengthening of the hip rotators is a frequently used rehabilitation program. Another program contains strengthening of the hamstrings and gluteal muscles by climbing stairs and reverse curls.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.