Paraplegia results from spinal cord injury (SCI) affecting the lower limbs, leading to motor and sensory impairments. Rehabilitation aims to restore maximum independence, prevent complications, and enhance the patient’s quality of life through a structured Rehabilitation Protocol for Paraplegic Patients.
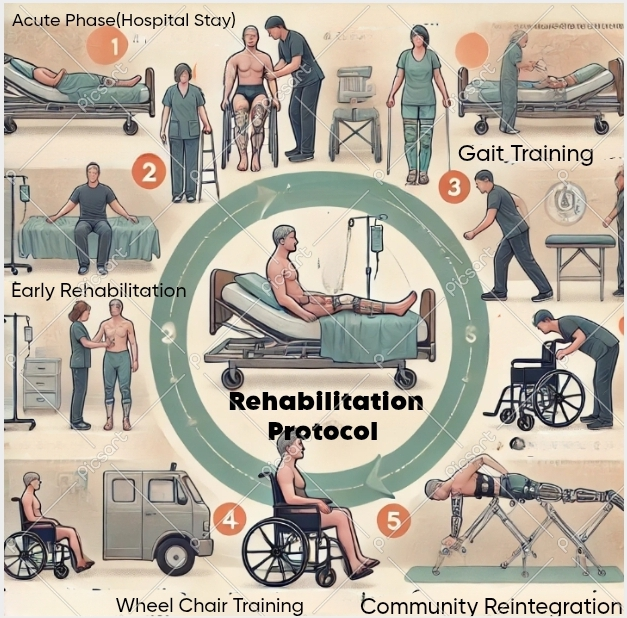
1. Acute Stage (0-6 Weeks Post-Injury):
Goals:
– Stabilize the patient medically and neurologically.
– Prevent secondary complications (pressure ulcers, deep vein thrombosis, infections).
– Maintain joint mobility and muscle function in unaffected areas.
– Begin early psychological and social support.
Medical Management:
Spinal Cord Stabilization:
– Surgical intervention (spinal decompression or fixation) if needed.
– Non-surgical management with immobilization (bracing, traction).
Pain Control:
– Opioids for acute pain.
– Neuropathic pain medications (gabapentin, pregabalin) for nerve-related discomfort.
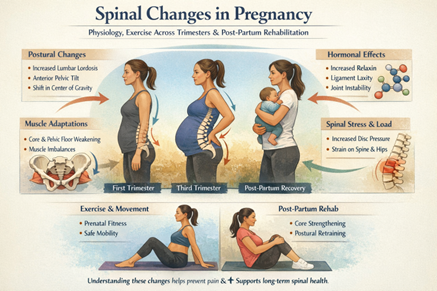
Respiratory Care:
– Breathing exercises to prevent pneumonia.
– Assisted coughing techniques for weak expiratory muscles.

Cardiovascular Support:
– Prevention of orthostatic hypotension with gradual mobilization and abdominal binders.
– Compression stockings and anticoagulants to reduce the risk of deep vein thrombosis (DVT).
Bladder and Bowel Management:
Bladder: Intermittent catheterization to prevent infections and urinary retention.
Bowel: A bowel program with dietary fiber, stool softeners, and digital stimulation.
Early Physical Rehabilitation:
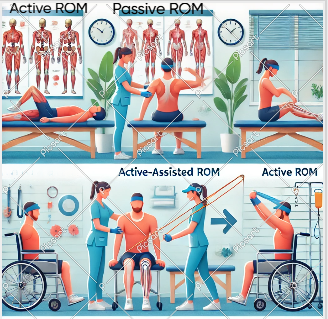
Passive & Active-Assisted Range of Motion (ROM) Exercises:
– Prevent joint stiffness and muscle contractures.
– Maintain circulation and reduce the risk of deep vein thrombosis.
Bed Mobility & Positioning:
– Frequent repositioning every 2 hours to avoid pressure ulcers.
– Elevation of lower limbs to prevent swelling.
Sitting Balance Training:
– Use of a tilt table to introduce upright positioning.
– Gradual increase in wheelchair sitting tolerance.
Upper Limb Strengthening:
– Focus on shoulders, arms, and core to prepare for wheelchair use and transfers.
2. Chronic Stage (Beyond 6 Weeks – Long-Term Rehabilitation):
Goals:
– Maximize independence in daily activities.
– Strengthen muscles for wheelchair mobility.
– Prevent long-term complications like osteoporosis and contractures.
– Support psychological and social reintegration.
Physical Therapy and Functional Training:
Strengthening Exercises:
– Upper limb exercises to improve wheelchair propulsion and self-transfers.
– Core strengthening to enhance posture and stability.
Wheelchair Training:
– Proper propulsion techniques to avoid shoulder overuse injuries.
– Navigating ramps, curbs, and uneven terrain safely.
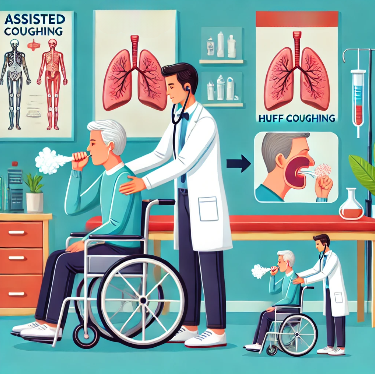
Standing & Walking Aids (if applicable):
– Standing frames or orthotic devices (e.g., knee-ankle-foot orthoses – KAFOs).
– Bodyweight-supported treadmill training (BWSTT) or robotic-assisted gait therapy.

Hydrotherapy (Aquatic Therapy):
– Reduces joint stress and improves muscle strength.
– Facilitates movement in a gravity-reduced environment.
Occupational Therapy for Daily Activities:
– Training in Activities of Daily Living (ADLs) such as dressing, grooming, and cooking.
– Adaptive tools like grab bars, long-handled reachers and voice-activated controls.
– Home modifications for accessibility (ramps, wider doorways, bathroom adaptations).
Psychological & Social Support:
– Counseling to manage depression, anxiety, and emotional distress.
– Support groups and vocational rehabilitation to reintegrate into society.
– Education on sexual health, fertility, and relationship adjustments.
3. Bed Sore (Pressure Ulcer) Management & Prevention:
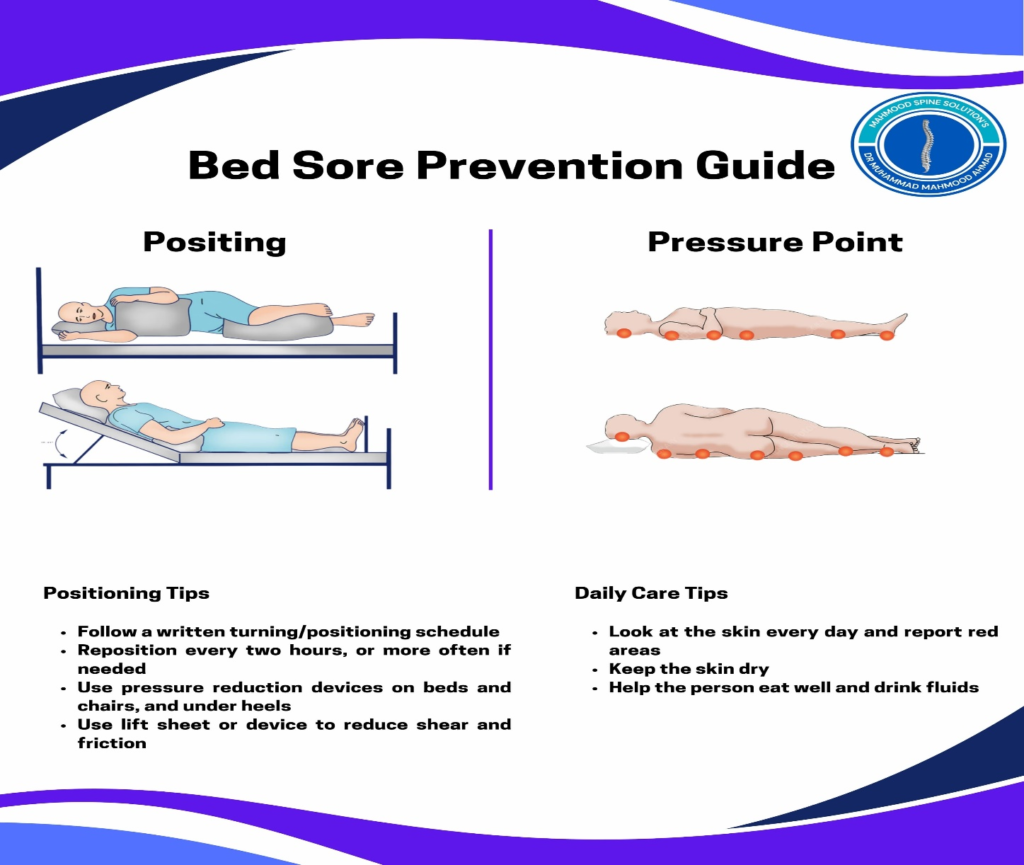
Preventive Strategies:
- Frequent Repositioning:
– In Bed: Change position every 2 hours to relieve pressure on bony areas.
– In Wheelchair: Perform weight shifts every 15-30 minutes (forward lean, side leans).
- Skin Inspection & Care:
– Daily examination of heels, sacrum, elbows, and hips for redness or skin breakdown.
– Keep skin clean, dry, and moisturized to prevent cracking.
- Pressure-Relieving Surfaces:
– Use high-density foam or air cushions for wheelchairs.
– Low-air-loss or alternating pressure mattresses for bed-bound patients.
- Proper Nutrition & Hydration:
– A high-protein diet supports wound healing.
– Adequate hydration prevents skin dryness and breakdown.
- Clothing & Bedding Considerations:
– Soft, breathable fabrics to reduce friction.
– Avoid wrinkled sheets and tight clothing that may cause pressure points.
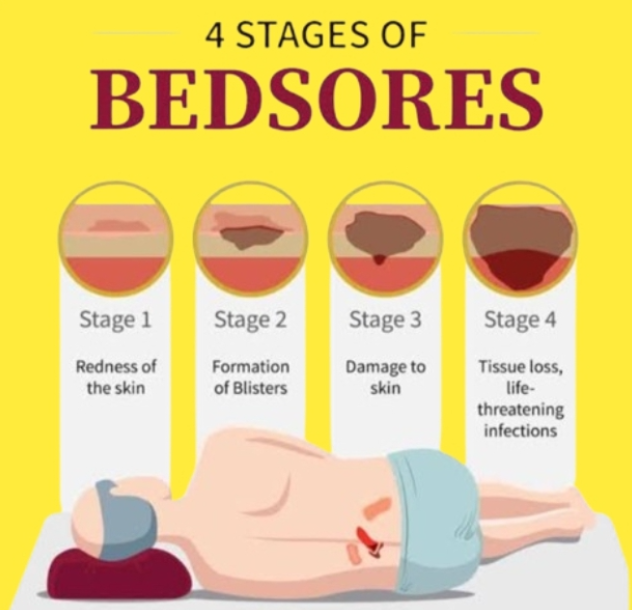
Treatment of Existing Bed Sores:
Stage 1 (Red, Intact Skin):
– Keep the area dry and clean.
– Use barrier creams (zinc oxide, petroleum jelly).
Stage 2 (Blistered or Open Skin):
– Apply hydrocolloid dressings to promote healing.
– Use antibiotic ointments if infection is suspected.
Stage 3 (Deeper Wound Exposing Fat Tissue):
– Require debridement to remove dead tissue.
– Use foam dressings or negative-pressure wound therapy.
Stage 4 (Deep Wound Exposing Muscle or Bone):
– May require surgical intervention (flap closure or grafting).
– Advanced wound care with antiseptics and frequent dressing changes.
Conclusion:
A multidisciplinary approach is essential for paraplegic rehabilitation, involving physicians, physiotherapists, occupational therapists, nurses, and psychologists. The focus is on early intervention, mobility training, skin care, and mental health support to ensure a better quality of life for the patient.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.