Facet joint syndrome, also known as facet arthritis, is an arthritis-like condition of the spine that can be a significant source of back and neck pain. It is caused by degenerative changes to the joints between the spine bones. The breakdown of cartilage inside the facet joint can lead to inflammation, triggering pain signals in nearby nerve endings and affecting spinal alignment. Understanding this condition is essential for managing symptoms and promoting spinal health.
What is happening anatomically?
- The joint surfaces are lined with cartilage allowing them to glide easily over each other. As we age, the cartilage gradually wears away, and in many cases, growth called “bone spurs” can develop.
- When a joint is damaged through normal deterioration, injury, or repetitive trauma, it may become swollen, painful, and stiff. Inflammation is usually temporary, but in arthritic joints, it may cause long-lasting or permanent disability.
- Abnormal bony growths, called osteophytes or bony spurs develop on the vertebrae.
- Bone spurs grow from the facet joints and rub against the nerves of the transverse foramen.
What happens Biomechanically?
- Friction between the bones leads to the tenderness, swelling, and pain of arthritis.
- Osteoarthritis or degeneration of a facet joint.
- The degradation and wear on the cartilage between the facet joints causes osteoarthritis.
Grades of Facet Arthritis:
Grade 0: No narrowing, sclerosis, or osteophytes.
Grade 1: Joint space narrowing or irregularity.
Grade 2: Narrowing plus sclerosis or hypertrophy with osteophyte formation.
Grade 3: Complete narrowing, sclerosis, and severe osteophyte formation.
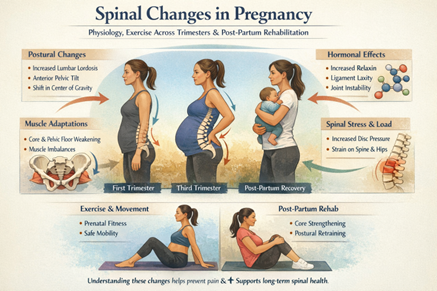
Causes:
- Aging
- Trauma (injury) and fractures to the spine.
- Degenerative disc disease.
- Family history of osteoarthritis.
- Being overweight or obese.
- Poor posture.
- Repetitive bending or twisting.
- Sedentary lifestyle.
Signs and Symptoms:
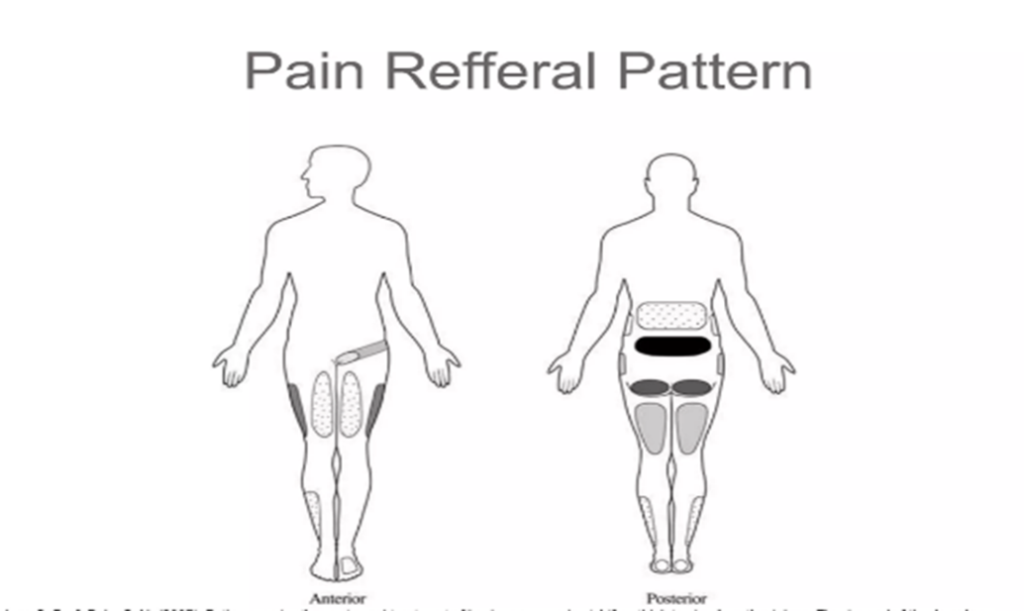
- Pain: The most common and noticeable symptom of facet arthritis is pain. Features of pain caused by facet arthritis include:
- Pain that is worse following sleep or rest.
- Lower back pain that worsens when twisting, bending backward, and standing.
- Pain centered on one specific area of the spine.
- A dull ache on one or both sides of the lower back.
- Development of other conditions including bone spurs, and spinal stenosis.
Differential Diagnosis:
- Facet Cyst
- Ankylosing Spondolysis
- Lumbar herniated disc
- Discogenic pain syndrome
- Lumbosacral radiculopathy
Diagnostic Test:
The Kemp test (also known as the quadrant test and extension-rotation test) is a provocative test useful for diagnosing pain related to facet joint pathology, e.g. osteoarthritis. The client performs combined extension and rotation of the spine (used for the cervical spine or the lumbar spine). The test is considered positive when the patient reports pain, numbness, or tingling in the area concerned.
Technique:
Standing position:
- The patient is standing before the therapist.
- The therapist fixes the opposite ilium from the side being tested with one hand.
- The other hand grabs the shoulder from the patient and leads the patient to extension, ipsilateral side bending, and rotation (3D extension movement).
- Hold this position for three seconds.
Seated Position:
- The patient was seated with arms crossed over the chest.
- One hand of the therapist stabilizes the patient’s lumbosacral region on the side to be tested.
- The other arm controls the patient’s upper body movement.
- The patient is passively directed into flexion, rotation, lateral flexion, and finally extension.
- Depending on the patient’s response, axial compression may be applied in the fully extended and rotated position to increase stress on the posterior joints.
- The test is positive when the patient reports pain, numbness or tingling in the area of the back or lower extremities.
Physical Therapy Protocol
Phase I
Precautions
- Keep the spine neutral for all strengthening and make sure to achieve proper neuromuscular control of transverse abdominis, multifidi before progressing strengthening exercises.
- If leg symptoms present, focus on centralizing pain out of the leg and do not progress strength exercises until achieved.
Goals
- Centralize symptoms out of the lower extremity (if present), then work to abolish if possible.
- Achieve proper muscle firing of transverse abdominis and multifidi, 10” each.
- Achieve proper muscle firing of glute muscles without substitution from hamstrings or lumbar paraspinal, 10” holds.
- Improve cardio endurance to at least 20 minutes, three to five days a week.
- Learn proper sitting posture with the lumbar roll and proper lifting mechanics.
Stabilization Exercises
- TA Bracing: 10” isometrics with normal breathing (without pelvic tilt) in supine, quadruped and prone.
- Multifidi:10” isometrics with normal breathing in prone
- Glute Sets: 10” isometrics with emphasis on proper glute firing in prone (bilateral and unilateral)
Directional Preference Exercises (repeated or static movements)
- If worse with flexion activities (sitting, bending, etc.), attempt extension exercises first and minimize flexion-based strengthening including pelvic tilts.
- If worse with extension activities (standing, walking, prone, etc.), attempt flexion exercises and neutral spine stabilization.
- If worse with both flexion and extension, work on exercises with a neutral spine and avoid end ranges.
Manual Therapy
- Sound-assisted soft tissue mobilization/augmented soft tissue mobilization as needed for areas of soft tissue restriction or muscle guarding.
- Address any positional faults with mobilization or contract/relaxation techniques.
- Joint mobilizations as needed.
Flexibility
- Stretching: Hip flexors, hamstrings, gastro/soleus, quadriceps.
- Hip Range of Motion: Restore normal extension, internal rotation, and external rotation if not within normal limits (mobilizations if needed).
Cardio (as long as it doesn’t produce or increase symptoms, let pain be the guide)
- Stationary bike, walking, swimming.
Phase II
Goals
- Patient able to activate co-contraction of transverse abdominis and multifidi regularly during daily activities, especially in situations where they anticipate or experience pain or feel unstable.
- Restore normal hip range of motion for extension, internal rotation, and external rotation (if they are not within normal limits).
- Once the patient can complete the exercises and cardio below without production of pain during or after, continue to Phase III.
Transverse Abdominis/Multifidi Progressions
- Supine: Add upper extremity/lower extremity movements (eg.: marches, straight leg raises, upper extremity lift and lowers, etc.)
- Quadruped: Alternating upper extremity, alternating lower extremity, alternating upper extremity /lower extremity (bird-dog
- Sidelying: Clams, hip abduction, etc.
- Prone: Hip extension, alternating upper extremity/lower extremity lifts (avoid hyperextension)
- Bridging: Bridges, single-leg bridges, on a Swiss ball, etc.
- Balance: Static (eg.: single leg stance, tandem, etc.)
- Swiss Ball: No sit-ups, no twisting (eg.: wall squats, seated exercises, bridges, bird-dog, etc.)
Cardio
- Stationary bike, walking, elliptical, swimming, hiking, Pilates.
Phase III
Only initiate these once the patient can complete Phase II exercises correctly and without an increase in pain.
Transverse Abdominis /Multifidi Progressions
- Lower extremity strengthening with transverse abdominis bracing (lunges, squats, step-ups, etc.)
- Balance: Progress with BOSU, dynamic balance, etc.
- Swiss Ball: Advanced exercises (continue extension and rotation precautions)
Cardio
- Stationary bike, walking, elliptical, swimming, Pilates, hiking, running.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.