Myofascial trigger points (MTrPs) are hyperirritable nodules found within taut bands of skeletal muscle fibers, commonly associated with musculoskeletal pain syndromes, including neck pain. These trigger points can cause localized discomfort, referred pain, muscle stiffness, and limited range of motion. Dry needling (DN) is a minimally invasive therapeutic intervention that targets these MTrPs using fine, sterile needles without injecting any substance. This technique has gained popularity in musculoskeletal rehabilitation due to its effectiveness in reducing pain, improving function, and enhancing mobility.
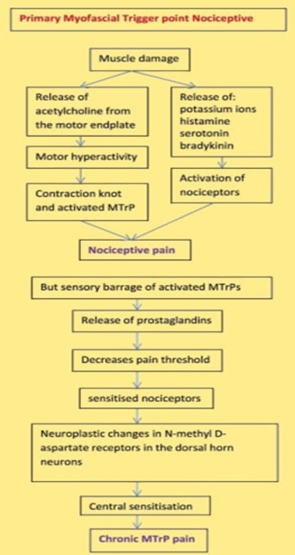
Mechanism of Action:
Dry needling involves the insertion of thin, solid filament needles into MTrPs, aiming to produce a local twitch response (LTR). The physiological mechanisms through which dry needling exerts its therapeutic effects include:
- Neuromuscular Modulation: Dry needling disrupts abnormal neuromuscular junction activity by reducing excessive acetylcholine release, which is associated with trigger point formation.
- Mechanical Disruption of MTrPs: The insertion of the needle mechanically disrupts the taut muscle band, leading to relaxation and improved muscle elasticity.
- Enhancement of Blood Flow and Oxygenation: Trigger points are often ischemic and hypoxic, contributing to pain and dysfunction. Dry needling increases local blood circulation, promoting oxygen and nutrient delivery to affected tissues.
- Pain Modulation via Endogenous Opioids and Descending Inhibitory Pathways: Dry needling stimulates sensory afferent pathways, leading to the activation of endogenous opioid release, thereby reducing pain perception.
- Reduction of Central and Peripheral Sensitization: Chronic myofascial pain conditions can involve central and peripheral sensitization. Dry needling may help modulate these pathways by decreasing nociceptive input from MTrPs.
Clinical Benefits of Dry Needling in Neck Pain Management
- Pain Reduction:
Studies indicate that dry needling effectively reduces pain intensity by deactivating MTrPs and decreasing peripheral nociceptive input. This effect is comparable to or even superior to manual therapy and other conservative treatments in certain cases.
- Improved Range of Motion (ROM) and Muscle Function:
Patients with neck pain often experience restricted movement due to muscle stiffness. Dry needling facilitates muscle relaxation and improves ROM, leading to better postural alignment and functional mobility.
- Decreased Muscle Spasm and Tension:
By targeting MTrPs, dry needling alleviates involuntary muscle contractions, reducing chronic muscle spasm and associated discomfort.
- Neuromuscular Re-Education and Motor Control:
Persistent neck pain can lead to maladaptive movement patterns and altered motor control. Dry needling helps restore proper neuromuscular function, particularly when combined with therapeutic exercises.
- Long-Term Functional Improvements:
Patients undergoing dry needling often report improved daily activities, reduced reliance on pain medication, and enhanced quality of life.
Comparison with Other Treatments:
Dry needling is frequently compared to other myofascial pain treatments such as manual therapy, massage, and trigger point injections. Unlike manual therapy, which relies on external pressure, dry needling directly targets the myofascial tissue. While trigger point injections involve the administration of anesthetic or corticosteroids, dry needling is a drug-free alternative with fewer systemic risks. Furthermore, when combined with physical therapy, dry needling has been shown to enhance rehabilitation outcomes.
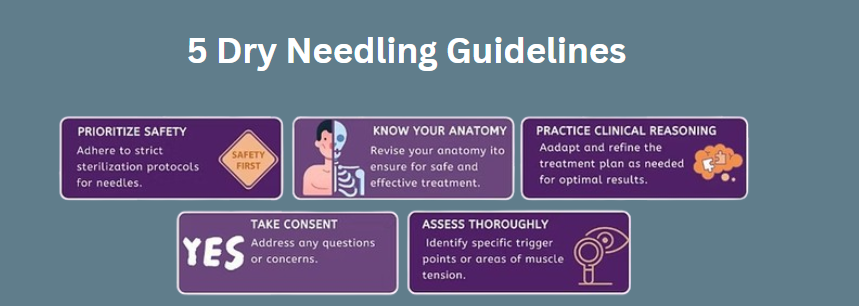
Safety Considerations and Potential Risks:
When performed by a trained healthcare professional, dry needling is a safe and well-tolerated procedure. However, some potential minor side effects include:
– Temporary soreness or bruising at the needling site
– Mild bleeding or hematoma formation
– Post-needling fatigue or dizziness
Rare but serious complications, such as pneumothorax, can occur if needling is performed in high-risk areas without proper anatomical knowledge. Therefore, clinicians must be adequately trained in dry needling techniques to ensure patient safety.
Conclusion:
Dry needling is an effective and evidence-based intervention for managing myofascial trigger points in patients with neck pain. It offers multiple therapeutic benefits, including pain relief, improved mobility, and neuromuscular function restoration. When integrated with a comprehensive treatment plan—such as physical therapy, stretching, and ergonomic modifications—dry needling can significantly enhance patient outcomes. Further research and clinical trials continue to support its efficacy, making it a valuable tool in musculoskeletal rehabilitation.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.