Diabetes mellitus is a chronic metabolic condition characterized by elevated blood glucose levels due to either insufficient insulin production or impaired insulin action. While its primary complications are often associated with cardiovascular, renal, and visual systems, musculoskeletal issues, including spine pain, are increasingly recognized but often underdiagnosed. This link has significant implications for physiotherapists in designing holistic and safe rehabilitation strategies.
Hidden Links Between Diabetes and Spine Pain:
1. Advanced Glycation End Products (AGEs):
Chronic hyperglycemia leads to the accumulation of AGEs in collagen-rich tissues like intervertebral discs and ligaments. These compounds:
- Increase disc stiffness
- Reduce disc hydration
- Promote early disc degeneration
→ Resulting in chronic low back or neck pain.
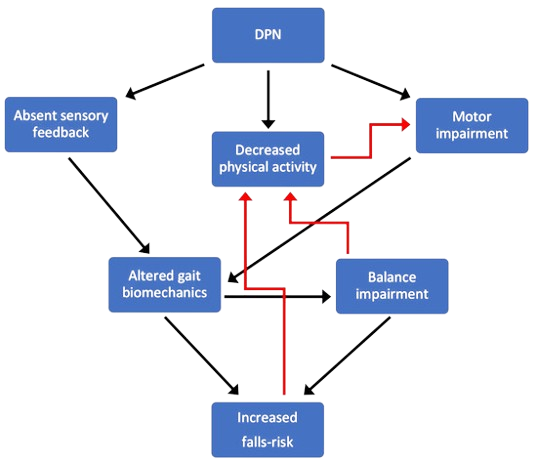
2. Neuropathy and Altered Biomechanics:
Peripheral neuropathy in diabetic patients:
- Impairs proprioception and balance
- Leads to poor posture and compensatory spinal movements
→ This can strain paraspinal muscles and cause pain over time.
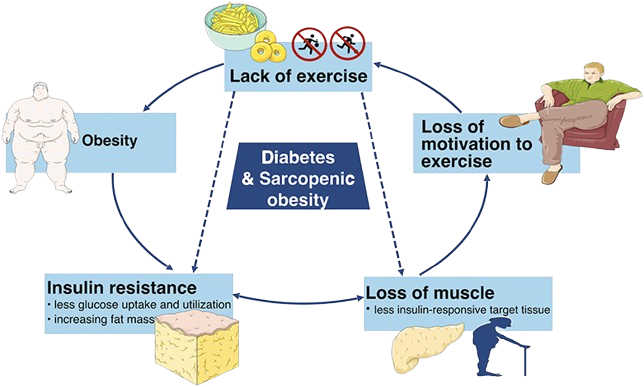
3. Obesity and Inflammation:
Many individuals with type 2 diabetes are also overweight. Excess body weight:
- Places additional mechanical load on the spine
- Increases systemic inflammation, which exacerbates pain and joint degeneration.
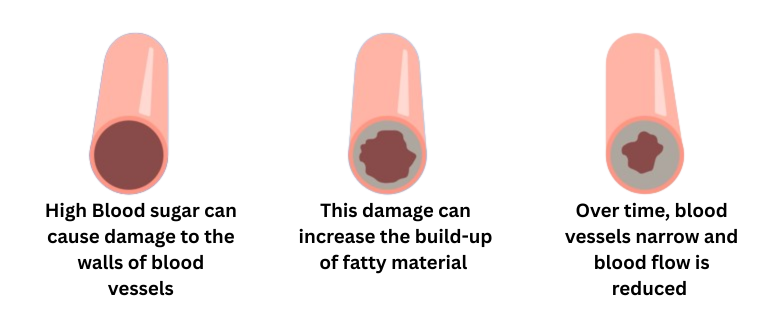
4. Microvascular Compromise:
Diabetes damages small blood vessels, reducing blood flow to spinal structures:
- Leads to tissue ischemia
- Contributes to degenerative changes and impaired healing
5. Reduced Physical Activity:
Pain, fatigue, and complications discourage movement, leading to deconditioning:
- Weak core and back muscles
- Increased susceptibility to musculoskeletal pain and spinal dysfunction
Physiotherapy Approaches for Spine Pain in Diabetic Patients:
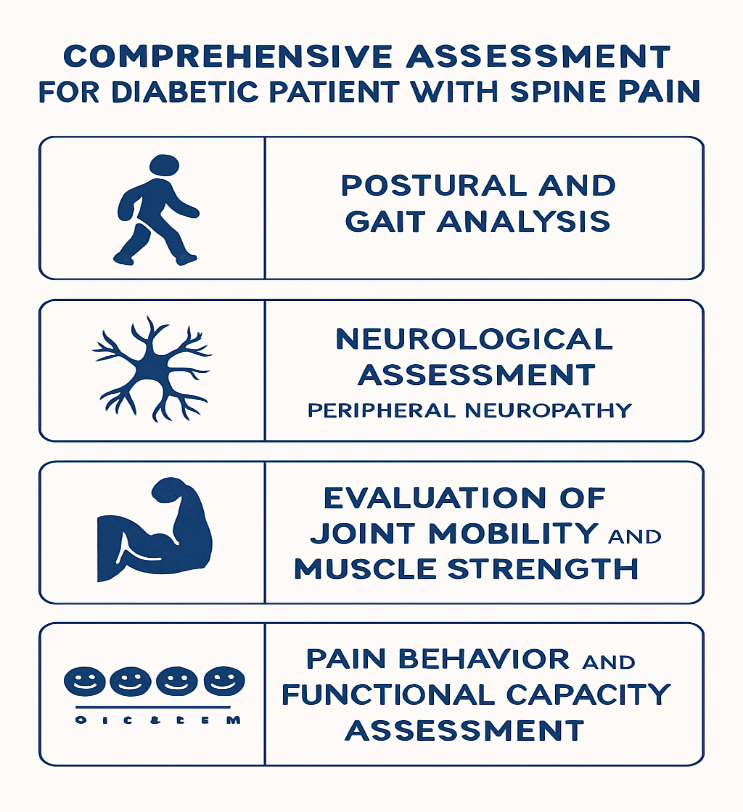
1. Comprehensive Assessment:
A diabetic patient with spine pain requires:
- Postural and gait analysis
- Neurological assessment (especially for peripheral neuropathy)
- Evaluation of joint mobility and muscle strength
- Pain behavior and functional capacity assessment
2. Education and Lifestyle Counseling:
- Educate the patient about safe physical activity
- Encourage regular blood glucose monitoring
- Teach body mechanics and ergonomic principles to reduce spinal load
3. Aerobic Exercise:
- Low-impact aerobic activities (e.g., walking, cycling, swimming)
- Improve cardiovascular health and insulin sensitivity
- Aids in weight control and reduces spine stress
4. Core and Postural Strengthening:
- Focus on core stabilization to support spinal structures
- Exercises like pelvic tilts, bridging, bird-dog, and modified planks
- Include postural correction routines to address alignment issues
5. Flexibility and Stretching:
- Gentle stretching for tight hamstrings, hip flexors, and back muscles
- Improve mobility and reduce muscular imbalances
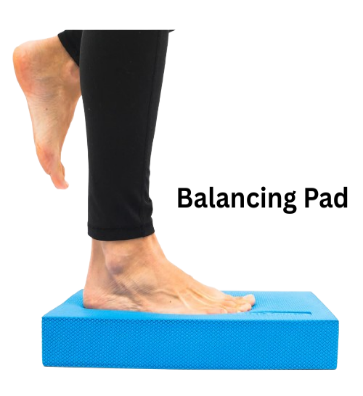
6. Balance and Proprioception Training:
- Especially for those with diabetic neuropathy
- Use wobble boards, balance pads, and closed-chain exercises
7. Manual Therapy (With Precaution):
- Soft tissue mobilization, myofascial release, and joint mobilization techniques
→ Should be used carefully, especially if the patient has decreased skin integrity or neuropathy
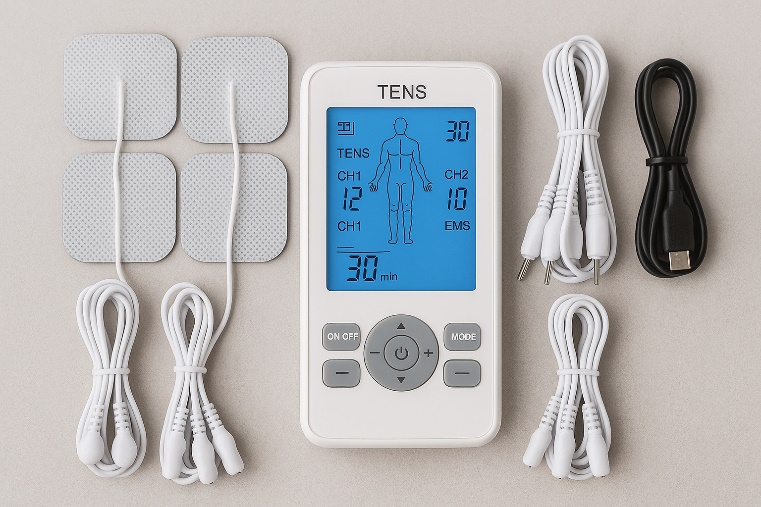
8. Electrotherapy Modalities:
- TENS (Transcutaneous Electrical Nerve Stimulation) for pain relief
- EMS (Electrical Muscle Stimulation) to maintain muscle function in case of inactivity
→ Use with caution in patients with peripheral vascular disease or sensory loss
9. Diabetic Foot and Lower Limb Management:
- Address any biomechanical issues in the lower limbs that might affect spinal alignment (e.g., orthotics for foot drop)
Precautions for Physiotherapists:
- Monitor for signs of hypoglycemia during sessions
- Ensure proper foot care and skin inspection
- Avoid aggressive mobilization if there is poor wound healing or severe neuropathy
- Schedule exercise when blood sugar levels are stable
Conclusion:
The relationship between diabetes and spine pain is complex and multifactorial, involving structural, neurological, vascular, and lifestyle factors. Physiotherapy plays a crucial role in alleviating pain, enhancing function, and improving the quality of life in diabetic patients. A tailored, cautious, and multi-dimensional approach is essential to manage spine pain in this population safely.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.