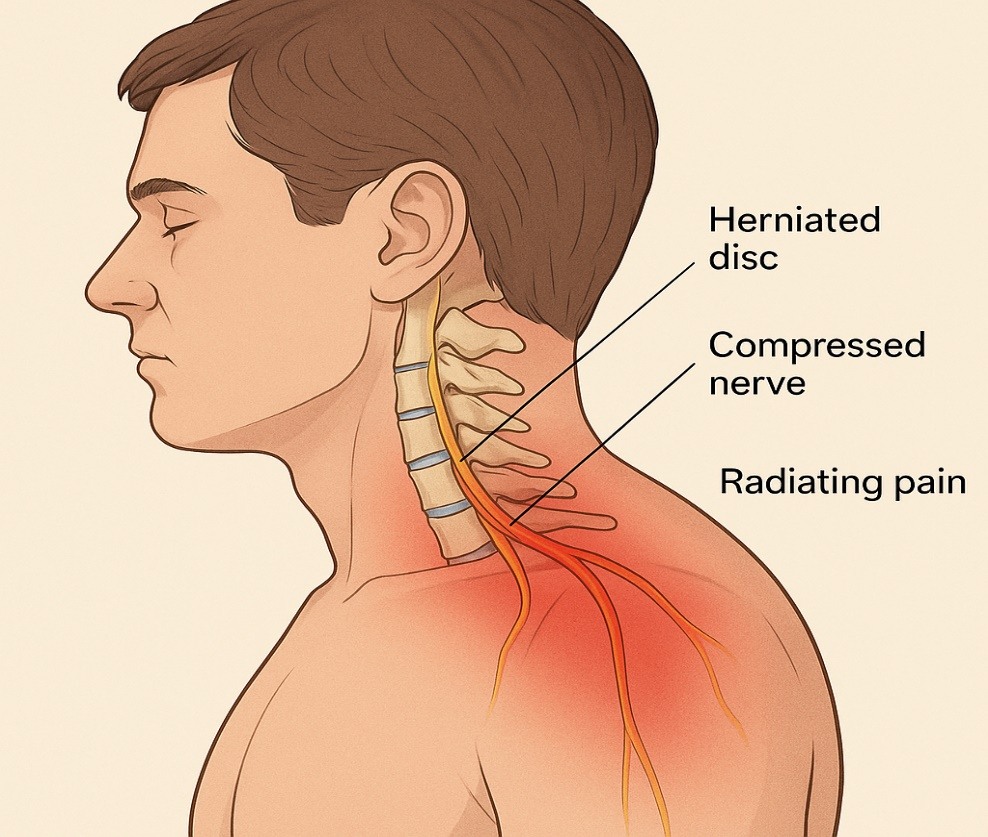
Cervical radiculopathy is a neurological condition characterized by dysfunction of a cervical spinal nerve root, typically due to compression or inflammation. This condition often manifests with pain, numbness, tingling, or weakness that radiates from the neck into the shoulder, arm, or hand. Common etiologies include cervical disc herniation, degenerative changes such as spondylosis, or foraminal narrowing secondary to osteophyte formation.
The role of physical therapy in managing cervical radiculopathy is crucial, as conservative interventions can often lead to significant symptomatic relief and functional recovery without the need for surgical intervention.
Clinical Presentation:
Patients with cervical radiculopathy may present with:
– Neck pain radiating to the upper extremity
– Sensory disturbances such as paresthesia or hypoesthesia in a dermatomal pattern
– Motor weakness corresponding to the affected myotomes
– Diminished or absent reflexes
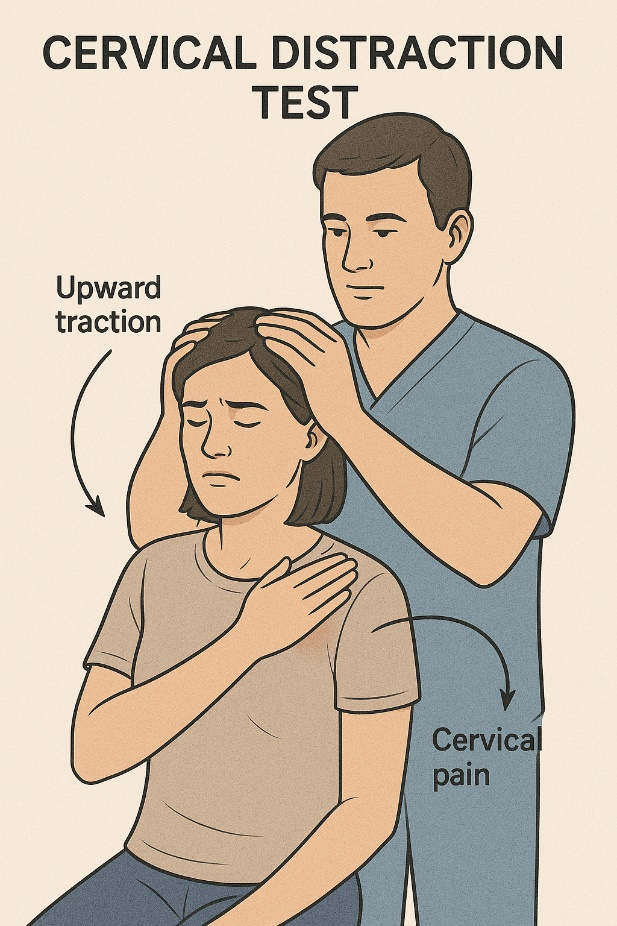
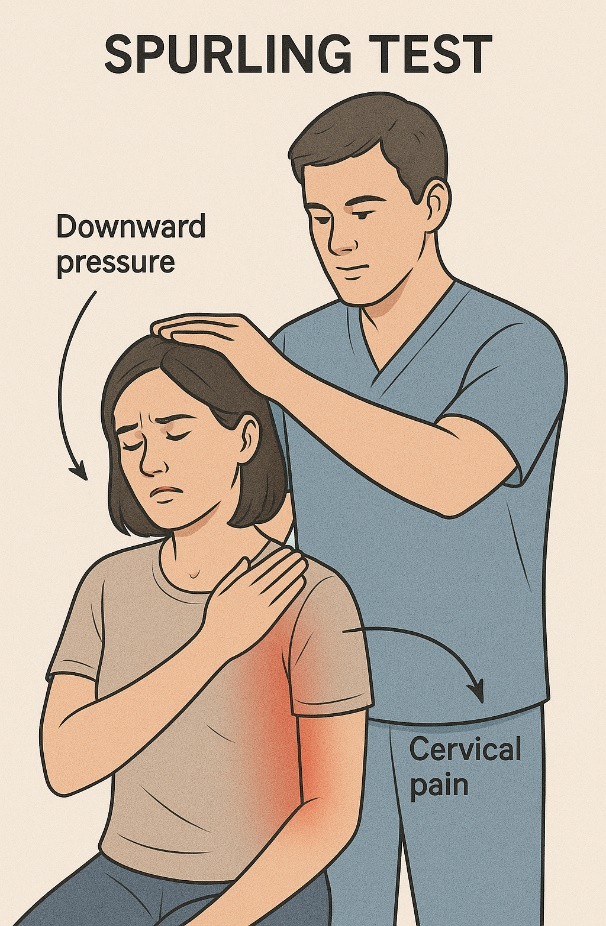
– Positive special tests such as Spurling’s test, cervical distraction test, and upper limb tension tests (ULTTs)
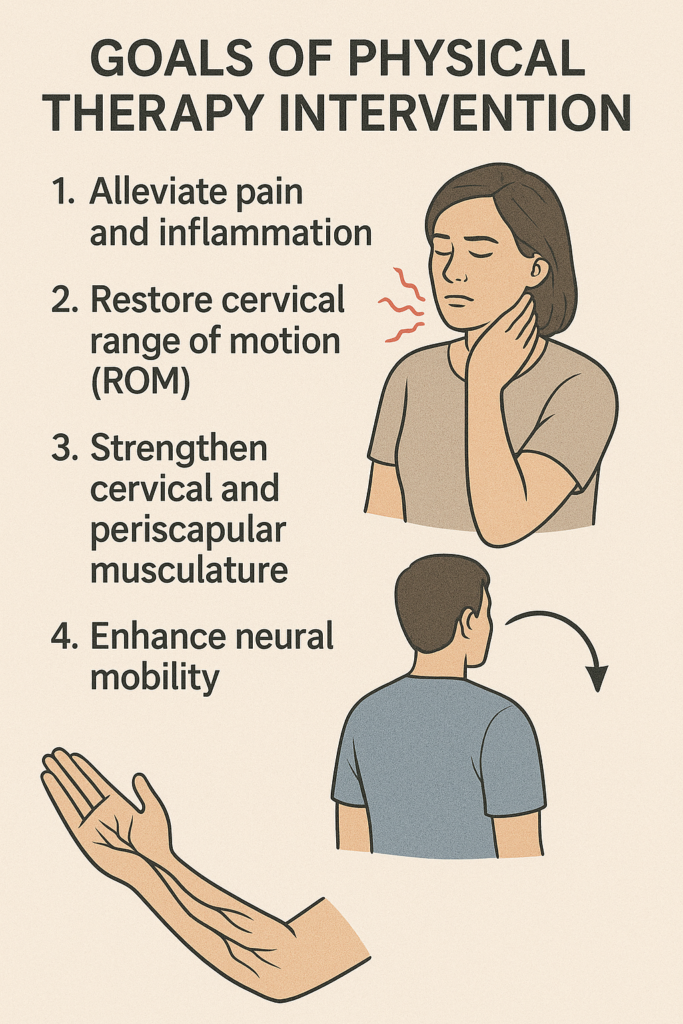
Goals of Physical Therapy Intervention:
The primary objectives of physical therapy in cervical radiculopathy are:
– Alleviate pain and inflammation
– Restore cervical range of motion (ROM) and segmental mobility
– Strengthen cervical and periscapular musculature
– Promote optimal postural alignment
– Enhance neural mobility
– Educate patients in self-management and recurrence prevention
Comprehensive Physical Therapy Assessment:
A thorough evaluation is vital to establish a baseline and create a tailored treatment plan. Key components include:
– Detailed patient history (onset, aggravating/relieving factors, previous interventions)
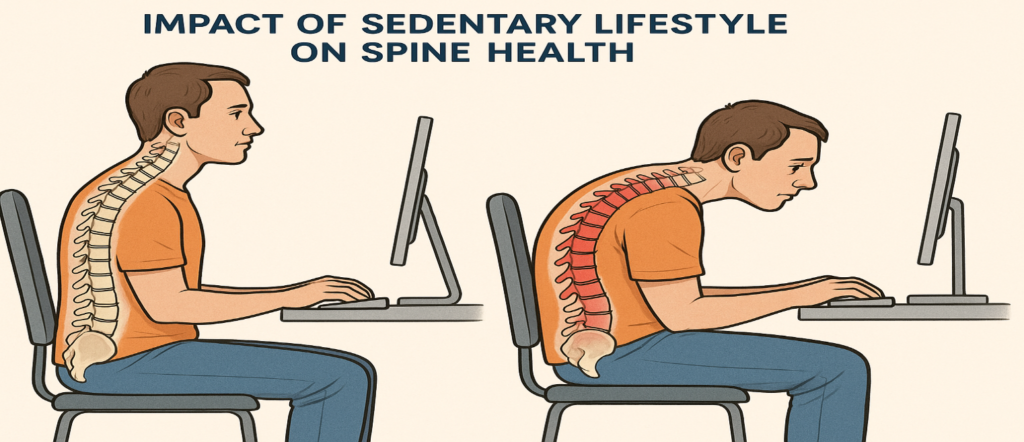
– Postural assessment
– Neurological examination: dermatomes, myotomes, reflex testing
– Cervical ROM and manual segmental mobility testing
– Special orthopedic tests (e.g., Spurling’s, distraction test, ULTTs)
– Pain assessment tools (VAS, NPRS)
– Functional outcome measures (e.g., Neck Disability Index)
Physical Therapy Management Strategies:
1. Pain Relief and Inflammation Control:
Activity Modification: Avoidance of provocative movements or postures
Modalities: Application of ice, heat, transcutaneous electrical nerve stimulation (TENS), and therapeutic ultrasound for symptomatic relief
Manual Therapy: Gentle cervical traction, soft tissue mobilization, and joint mobilizations aimed at reducing muscle tension and joint stiffness


2. Cervical Traction:
– Manual or mechanical traction can be beneficial in reducing nerve root compression and radicular symptoms.
– Initial parameters are typically low force (10–15 lbs), progressing based on patient response.
– Traction is especially useful when symptoms are aggravated by spinal loading and relieved with unloading.
3. Therapeutic Exercise Program:
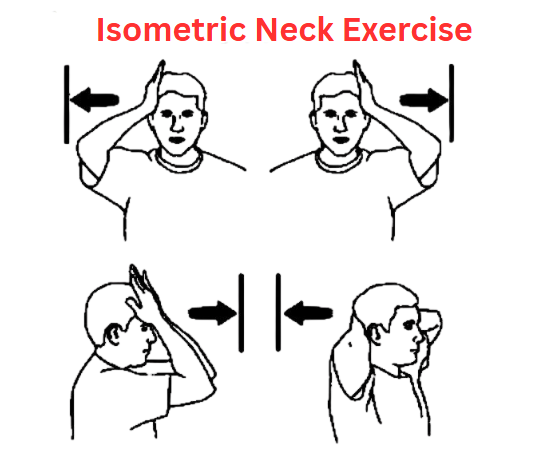
Acute Phase:
– Pain control and movement preservation
– Gentle cervical ROM exercises within pain-free range
– Isometric neck exercises
– Scapular setting and postural awareness drills
Subacute Phase:
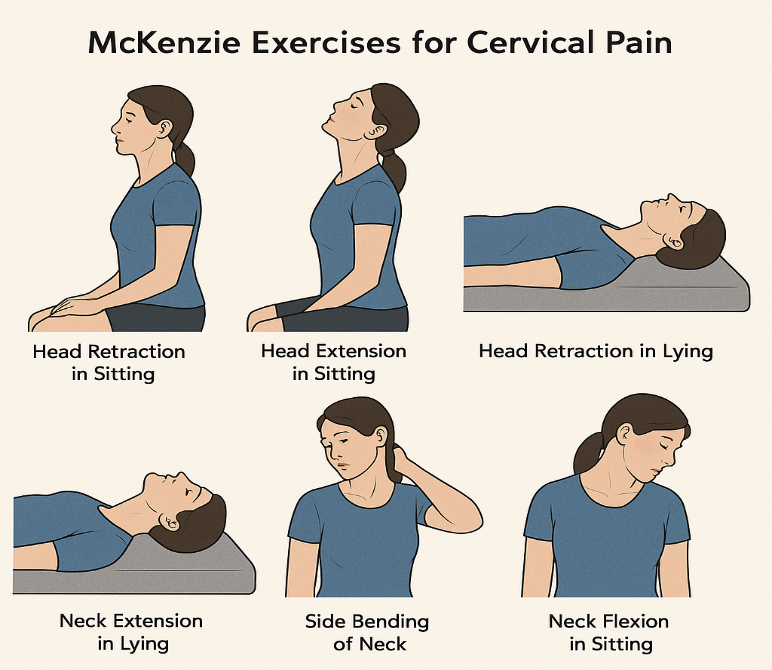
– McKenzie cervical retraction exercises to centralize symptoms
– Strengthening of deep neck flexors (e.g., chin tucks)
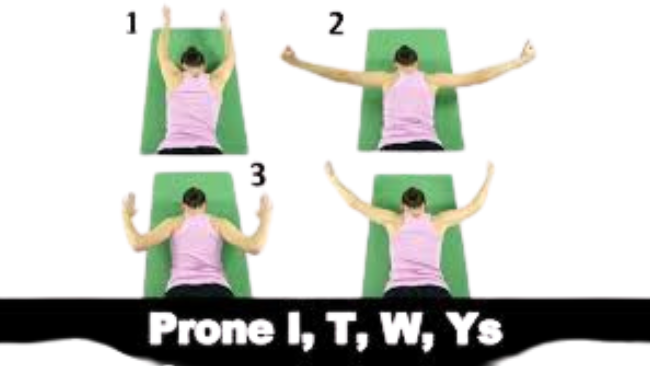
– Scapular and upper thoracic muscle reconditioning (e.g., rows, YTWs)
Chronic Phase:
– Progressive resistance training for neck and shoulder girdle
– Functional task training and dynamic stability exercises
– Proprioceptive neuromuscular facilitation (PNF) techniques for neuromuscular control
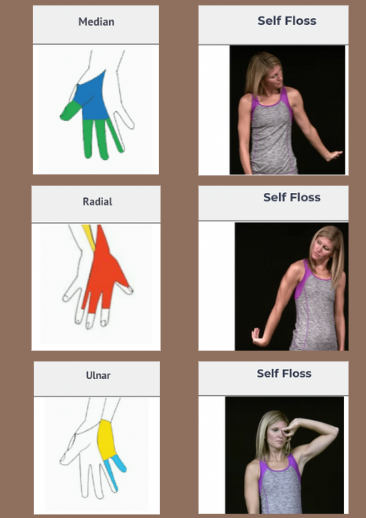
4. Neural Mobilization:
– Neural gliding or flossing techniques for the median, radial, or ulnar nerves are incorporated to address neurodynamic impairments without exacerbating symptoms.
5. Postural Correction and Ergonomic Education:
– Instruction on maintaining neutral spine posture during activities
– Ergonomic assessment of workplace or home environments
– Recommendations for sleep posture and appropriate pillow use
Patient Education:
Empowering the patient with knowledge is essential. Educational strategies should include:
– Explanation of condition and expected recovery timeline
– Importance of adherence to home exercise programs
– Avoidance of positions or activities that exacerbate symptoms
– Strategies for symptom management during flare-ups
When to Refer:
If the patient exhibits any of the following, referral to a physician or spine specialist is warranted:
– Progressive neurological deficits
– Symptoms persisting beyond 6–8 weeks of conservative care
– Signs of cervical myelopathy (e.g., balance disturbances, bowel/bladder dysfunction)
Conclusion:
Physical therapy plays a pivotal role in the conservative management of cervical radiculopathy. A structured and individualized rehabilitation program focusing on pain control, mobility restoration, postural correction, and neuromuscular strengthening can significantly improve patient outcomes. Interdisciplinary collaboration and timely referral are also essential components of comprehensive care.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.