What is Ankylosing Spondylitis?
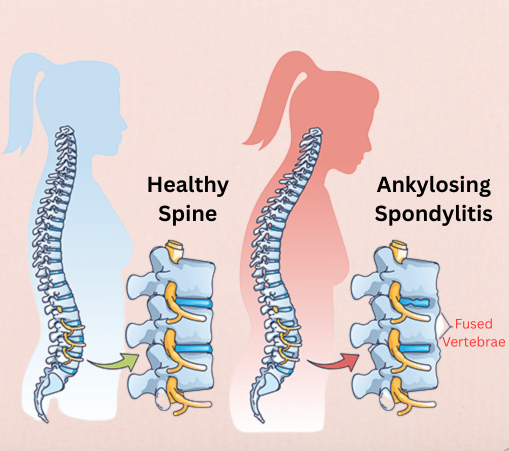
Ankylosing Spondylitis (AS) is a chronic, progressive inflammatory condition that primarily affects the spine and sacroiliac joints, leading to pain and stiffness. It belongs to a group of diseases known as spondyloarthropathies and is considered an autoimmune or autoinflammatory condition, where the body’s immune system mistakenly attacks its own tissues.
Over time, inflammation can lead to the fusion of vertebrae, resulting in a loss of spinal flexibility and a hunched posture. In severe cases, this fusion can significantly impact a person’s mobility and quality of life.
Causes and Risk Factors:
While the exact cause of Ankylosing Spondylitis is not fully understood, both genetic and environmental factors are involved.
Key Risk Factors Include:
Genetic Marker HLA-B27: Present in over 85–90% of individuals with AS.
Family History: A close relative with AS increases risk.
Age and Gender: Commonly begins in late adolescence or early adulthood, more prevalent in males.
Infections: Certain bacterial infections may trigger symptoms in genetically predisposed individuals.
Common Symptoms:
Symptoms usually develop gradually over weeks or months. Early recognition is crucial for preventing irreversible damage.
Initial Signs May Include:
- Chronic lower back pain, especially during rest or at night
- Morning stiffness that improves with activity
- Pain in the hips, buttocks, or shoulders
- Fatigue and general discomfort
As Disease Progresses:
- Restricted spinal movement
- Stooped or hunched posture (kyphosis)
- Pain in peripheral joints (knees, ankles)
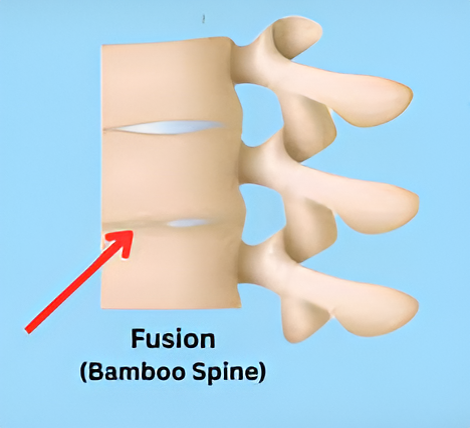
- In severe cases, fusion of vertebrae (bamboo spine)
Diagnosis:
Diagnosis is based on:
- Clinical history and physical examination
- Imaging (X-rays, MRI of sacroiliac joints)
- Blood tests (e.g., HLA-B27, ESR, CRP)
Early diagnosis can slow disease progression and prevent complications.
Medical Management:
While there is no cure, medical treatment focuses on controlling inflammation and maintaining function.
Common Treatment Options:
NSAIDs: First-line treatment to reduce pain and inflammation.
DMARDs: Disease-Modifying Anti-Rheumatic Drugs for joint symptoms.
Biologic Therapies: TNF-alpha inhibitors (e.g., etanercept, adalimumab) and IL-17 inhibitors (e.g., secukinumab).
Steroid Injections: For acute flare-ups in joints.
Physical Therapy Management:
Physical therapy is essential in the management of Ankylosing Spondylitis. Regular movement and targeted exercises can help maintain posture, reduce stiffness, and improve quality of life.
Goals of Physical Therapy:
- Improve spinal mobility and posture
- Maintain joint range of motion
- Reduce stiffness and muscle tightness
- Enhance breathing capacity (thoracic expansion)
- Support functional independence
Key Components of a Physical Therapy Program:
1) Postural Training:
- Encourage upright posture through awareness and alignment exercises.
- Use of mirrors or postural feedback tools.
2) Spinal Extension Exercises:
- Cat-cow stretch, prone press-ups, and wall angels to maintain extension and counteract kyphosis.
3) Stretching and Flexibility:
- Focus on hip flexors, hamstrings, chest, and back muscles.
- Gentle yoga poses can also be effective.
4) Breathing Exercises:
- Deep diaphragmatic breathing to improve lung expansion.
- Rib cage mobility is important as thoracic stiffness progresses.
5) Aerobic Conditioning:
- Low-impact activities such as swimming, walking, and cycling.
- Promotes cardiovascular health without stressing the joints.
6) Strength Training:
- Build muscle support around the spine and pelvis.
- Emphasis on core stability and pelvic control.
7) Hydrotherapy (Aquatic Therapy):
- Exercises in warm water reduce joint stress and improve flexibility.
8) Patient Education:
- Importance of regular activity
- Ergonomic advice for work and sleep
- Self-management during flare-ups
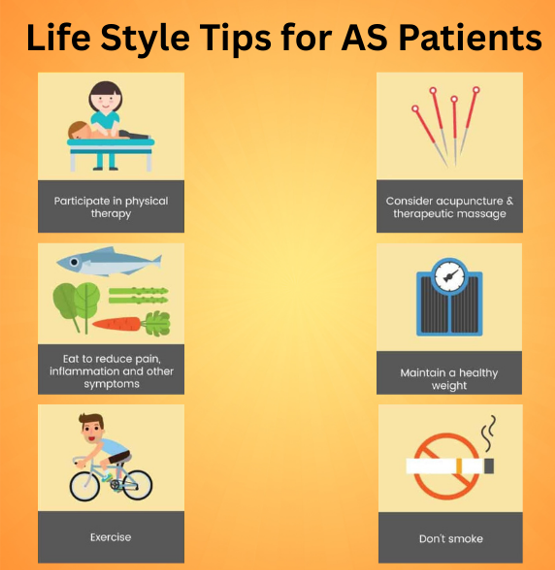
Lifestyle Tips for AS Patients:
- Avoid prolonged inactivity or sitting
- Maintain a healthy weight
- Use supportive footwear
- Sleep on a firm mattress in a spine-aligned position
- Avoid smoking, which worsens spinal damage
Conclusion:
Ankylosing Spondylitis is a life-altering condition, but with early diagnosis, medical treatment, and a structured physical therapy program, individuals can lead active and fulfilling lives. Physical therapy is not just a supportive measure—it is a core part of long-term AS management.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.