Introduction:
Pain is a complex and multifaceted experience that extends beyond physical sensations. It is influenced by biological, psychological, and social factors that shape how an individual perceives and responds to discomfort. In rehabilitation settings, understanding the role of psychological factors is crucial for effective pain management and recovery. Addressing these components not only improves treatment outcomes but also enhances patients’ overall quality of life.
Understanding Pain Perception:
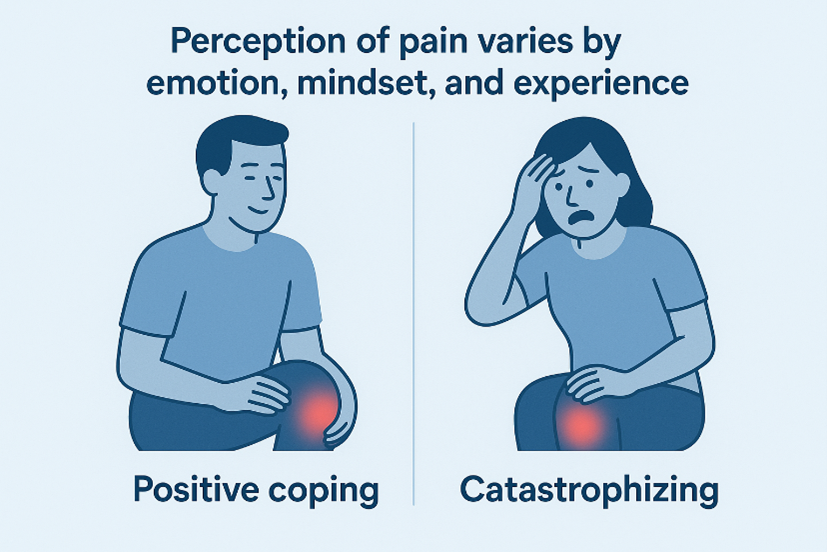
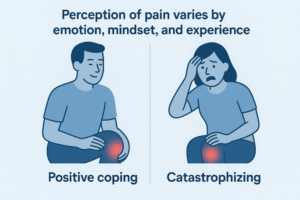
Pain perception is not a direct reflection of tissue damage but rather the brain’s interpretation of sensory signals from the body. The biopsychosocial model of pain highlights that emotional state, beliefs, and past experiences can significantly modify how pain is felt and expressed.
For example, two individuals with similar injuries may report vastly different pain intensities depending on their emotional resilience, coping strategies, and mental health status.
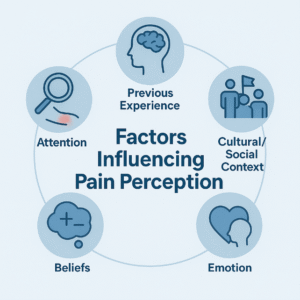
Key elements influencing pain perception include:
- Attention and focus: The more a person concentrates on pain, the more intense it feels.
- Previous experiences: Prior encounters with pain can heighten sensitivity or create fear of recurrence.
- Cultural and social context: Beliefs and attitudes toward pain vary across societies and affect pain expression.
Psychological Factors Affecting Rehabilitation:
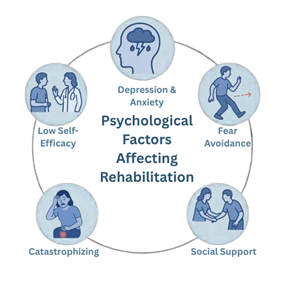
During rehabilitation, psychological factors play a determining role in how well a patient adheres to therapy and recovers. The following are among the most influential:
-
Fear-Avoidance Beliefs:
Patients who fear pain or re-injury often avoid physical activity, leading to muscle weakness, stiffness, and prolonged disability. Overcoming these fears through education and graded exposure is vital.
-
Depression and Anxiety:
Emotional distress can amplify pain perception by altering neurotransmitter activity in the brain. Depressed or anxious individuals may show slower progress and reduced motivation to participate in therapy.
-
Catastrophizing:
This refers to an exaggerated negative mindset about pain, where patients expect the worst outcomes. Catastrophizing increases perceived pain intensity and hinders engagement in rehabilitation exercises.
-
Self-Efficacy and Motivation:
A patient’s belief in their ability to manage pain and perform exercises directly influences recovery. High self-efficacy promotes adherence, resilience, and faster functional improvement.
-
Social Support:
Encouragement from family, friends, and healthcare providers enhances emotional stability and compliance with treatment plans. Conversely, social isolation can delay healing.
The Role of Psychological Interventions in Rehabilitation
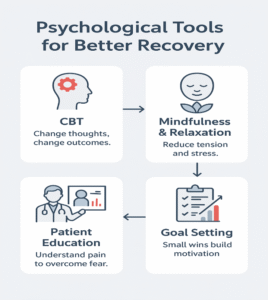
Integrating psychological approaches into physical rehabilitation can significantly improve outcomes. Common strategies include:
- Cognitive Behavioural Therapy (CBT): Helps modify unhelpful thoughts and behaviours related to pain.
- Mindfulness and Relaxation Techniques: Reduce stress, muscle tension, and pain sensitivity.
- Patient Education: Builds understanding of the pain mechanism, reducing fear and promoting active participation.
- Goal Setting and Positive Reinforcement: Encourages progress and maintains motivation throughout the recovery process.
Conclusion:
Pain is not merely a physical sensation—it is a dynamic experience shaped by psychological and emotional states. In rehabilitation, addressing psychological factors such as fear, anxiety, depression, and motivation is as essential as treating the physical condition itself. A holistic approach that integrates mental and physical therapies empowers patients to regain control, enhances adherence, and leads to more successful and lasting recovery outcomes.