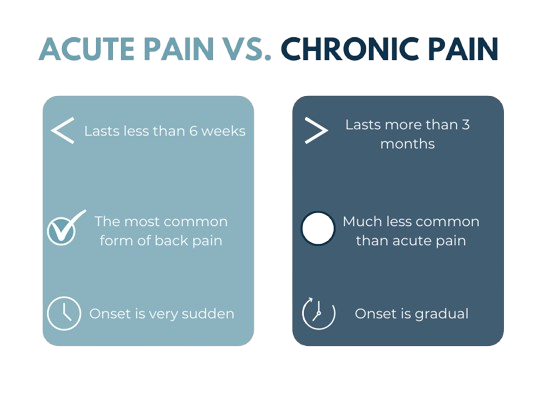
Back pain can vary greatly in intensity, location, and impact on daily life. Medical professionals often classify it into acute and chronic categories based on how long the pain lasts and the underlying causes. This distinction is important because the approach to diagnosis, treatment, and prevention can differ significantly.
Acute Back Pain
Acute back pain is sudden in onset and generally lasts less than six weeks. It is often related to a specific incident or injury.
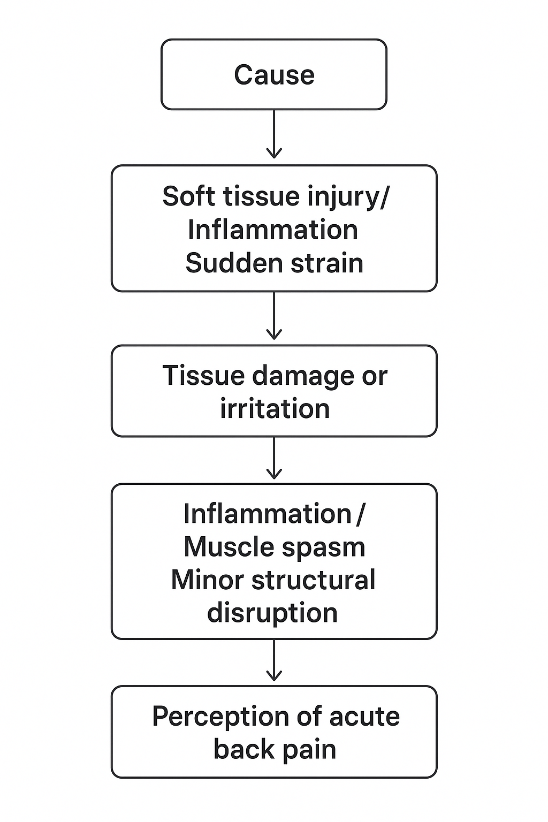
Mechanism:
- Usually caused by soft tissue injury, inflammation, or sudden strain.
- The pain is a signal from the body indicating that tissues have been damaged or irritated.
- Inflammation, muscle spasm, or minor structural disruption trigger pain receptors in the area.
Common Causes:
Mechanical strain: Lifting heavy objects with improper form, twisting suddenly.
Sports injuries: Sudden movements or impact during physical activity.
Postural stress: Sitting or standing in awkward positions for prolonged periods.
Minor trauma: Slips, trips, or falls.
Sudden movements: Rapid bending or reaching.
Risk Factors:
- Weak core and back muscles
- Poor lifting technique
- Sedentary lifestyle
- Sudden increase in activity without proper conditioning
Symptoms:
- Sharp, stabbing, or aching pain localized in the affected area.
- Pain may radiate slightly but usually remains in the lower back.
- Stiffness and reduced range of motion.
- Symptoms typically improve within days to weeks.
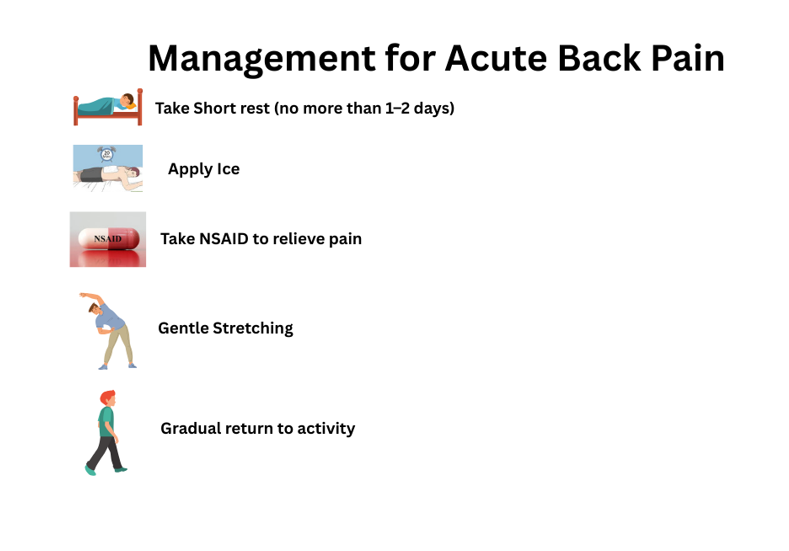
Management:
- Short rest (no more than 1–2 days) to prevent stiffness.
- Apply ice for the first 48 hours to reduce inflammation, followed by heat to relax the muscles.
- Over-the-counter pain relief (e.g., NSAIDs).
- Gentle stretching and gradual return to activity.
- Avoid prolonged bed rest, as movement aids recovery.
Prognosis:
Most cases resolve within a few weeks with conservative management. Persistent pain beyond this period may require further evaluation.
Chronic Back Pain
Chronic back pain persists for 12 weeks or longer, even if the initial injury or cause has been treated.
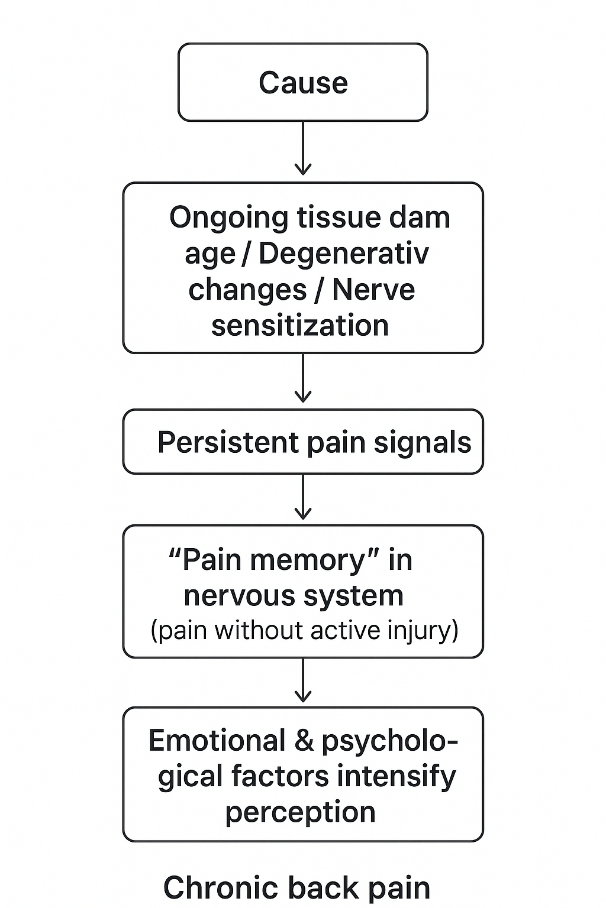
Mechanism:
- Pain signals continue due to ongoing tissue damage, degenerative changes, or nerve sensitization.
- In some cases, the nervous system remains in a “pain memory” state, where it continues to send pain signals without an active injury.
- Emotional and psychological factors may intensify pain perception.
Common Causes:
Degenerative changes: Osteoarthritis, degenerative disc disease.
Spinal structural issues: Spinal stenosis, herniated discs.
Nerve-related pain: Sciatica, nerve root compression.
Chronic conditions: Fibromyalgia, ankylosing spondylitis.
Post-surgical pain: Persistent discomfort after spinal surgery.
Risk Factors:
- Advancing age (wear and tear of spinal structures).
- Repetitive strain at work or during sports.
- Obesity (extra pressure on spinal structures).
- Smoking (reduces blood flow to spinal tissues).
- Untreated acute back pain that progresses.
Symptoms:
- Dull, deep, or burning pain, often persistent.
- May radiate to buttocks, legs, or other areas (radicular pain).
- Stiffness, muscle weakness, and reduced mobility.
- It can affect mood, sleep, and overall quality of life.
Management:
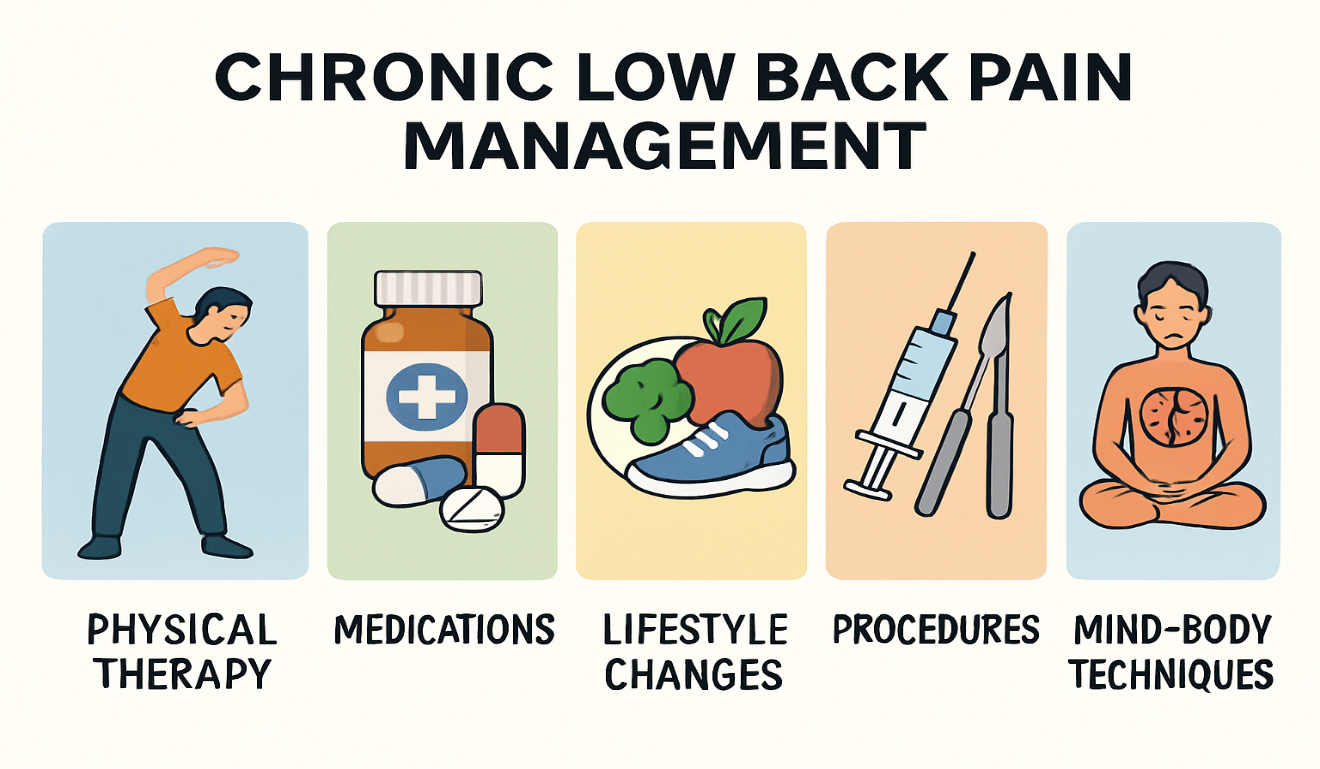
Multidisciplinary approach combining:
Physical therapy: Core strengthening, posture training.
Medications: NSAIDs, muscle relaxants, nerve pain agents.
Lifestyle changes: Weight management, ergonomic adjustments.
Interventional procedures: Nerve blocks, epidural injections.
Mind-body techniques: Cognitive-behavioral therapy, mindfulness.
Surgery is considered only when other treatments fail and a structural cause is identified.
Prognosis:
Chronic back pain may not fully resolve, but it can often be managed effectively with consistent treatment and preventive strategies.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.