Back pain is one of the most common complaints among people of all ages. One of the leading causes of back pain is disc herniation, a condition affecting the intervertebral discs that cushion the vertebrae in the spine. Disc herniation can cause a range of symptoms, from mild discomfort to severe pain, depending on its type and severity.
In this article, we’ll explore the four types of disc herniation, their symptoms, causes, and available treatments. By understanding these, you can make informed decisions about your health and seek timely medical intervention when needed.
What is Disc Herniation?
Disc herniation occurs when the gel-like center of an intervertebral disc (nucleus pulposus) pushes through the tougher outer ring (annulus fibrosus). This can put pressure on nearby nerves, leading to pain, numbness, or weakness. Depending on the extent and location of the herniation, the condition can range from mild to severe.
Disc herniation is often the result of age-related wear and tear, known as disc degeneration, but it can also occur due to injury, poor posture, or heavy lifting.
The 4 Types of Disc Herniation
Disc herniation is categorized into four main types based on the extent of displacement and damage to the disc structure. These types fall under PLID types (Posterolateral Intervertebral Disc types), which help to categorize the different forms of herniation. Let’s examine each type in detail.
1. Bulging Disc
Definition:
A bulging disc is the mildest form of disc herniation. It occurs when the nucleus pulposus remains intact but pushes against the annulus fibrosus, causing the disc to protrude outward.
Key Characteristics:
- The outer layers of the disc remain unbroken.
- The bulge often affects a large portion of the disc.
- This condition is common with age-related degeneration.
Symptoms:
- Many people with bulging discs experience no symptoms.
- If symptoms occur, they may include mild pain, stiffness, or discomfort in the back.
Why It Matters for Your Spine Health:
A bulging disc is often a precursor to more severe types of herniation if left untreated. It’s important to address the issue early with proper posture, regular exercise, and physical therapy.
2. Protrusion
Definition:
Protrusion occurs when the nucleus pulposus pushes outward but is still contained within the annulus fibrosus.
Key Characteristics:
- The disc shows significant deformation but remains intact.
- It typically occurs on one side, often compressing nearby nerves.
Symptoms:
- Localized back pain.
- Nerve-related symptoms such as tingling, numbness, or a burning sensation in the limbs.
Treatment Options:
Physical therapy and non-steroidal anti-inflammatory drugs (NSAIDs) are common treatments. Protrusion can often be managed effectively without surgery.
3. Extrusion
Definition:
Extrusion happens when the nucleus pulposus breaks through the annulus fibrosus but remains connected to the main disc structure.
Key Characteristics:
- The herniation extends beyond the disc’s outer layers.
- It often results in significant nerve compression.
Symptoms:
- Intense back pain that may radiate to the arms or legs.
- Neurological symptoms such as muscle weakness or loss of reflexes.
When to Seek Help:
Extrusion is a more advanced form of herniation that requires medical attention. If left untreated, it can lead to chronic pain or permanent nerve damage.
4. Sequestration
Definition:
Sequestration is the most severe form of disc herniation. In this case, fragments of the nucleus pulposus completely break away and move into the spinal canal.
Key Characteristics:
- Detached fragments may migrate and cause unpredictable symptoms.
- This condition poses a high risk of nerve damage.
Symptoms:
- Severe pain, often sudden and debilitating.
- Significant neurological issues such as numbness, tingling, or weakness.
- In extreme cases, loss of bowel or bladder control (a medical emergency known as cauda equina syndrome).
Why Early Diagnosis is Crucial:
Sequestration requires immediate medical attention. Treatment often involves surgery to remove the displaced fragments and relieve nerve compression.
Common Causes of Disc Herniation
Understanding the causes of disc herniation can help in preventing it. Below are some of the main factors:
- Age-Related Degeneration: Over time, intervertebral discs lose water content and elasticity, making them prone to damage.
- Injury: Sudden trauma, such as a fall or car accident, can lead to disc herniation.
- Poor Posture: Prolonged sitting, slouching, or incorrect lifting techniques can strain the spine.
- Repetitive Strain: Jobs or activities that involve repetitive bending, twisting, or heavy lifting.
- Genetics: A family history of disc problems can increase the risk.
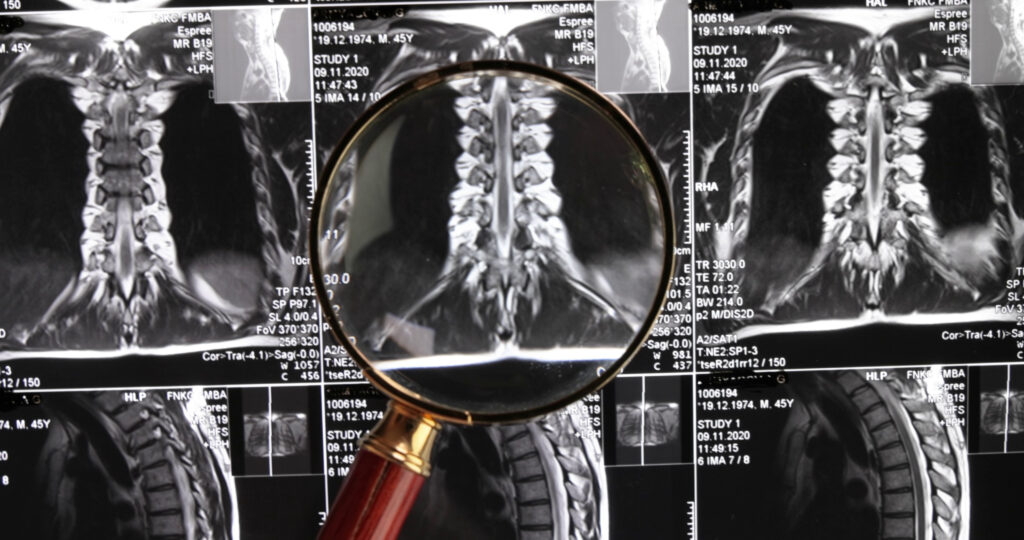
Diagnosing Disc Herniation
If you suspect disc herniation, a healthcare professional will perform the following:
- Physical Examination: Checking for pain, muscle weakness, and reflexes.
- Imaging Tests: MRI scans are the gold standard for diagnosing disc herniation as they provide detailed images of the spine. X-rays or CT scans may also be used.
- Nerve Tests: Electromyography (EMG) can assess nerve function and determine the extent of compression.
Treatment Options for Disc Herniation
Treatment depends on the type and severity of herniation:
Non-Surgical Treatments
- Physical Therapy: Strengthening and stretching exercises to reduce pressure on the spine.
- Medications: NSAIDs, muscle relaxants, and corticosteroids can help manage pain and inflammation.
- Lifestyle Changes: Improving posture, losing weight, and quitting smoking can reduce strain on the spine.
- Epidural Injections: Cortisone injections can provide temporary relief from nerve-related symptoms.
Surgical Treatments
If conservative treatments fail, surgery may be required:
- Microdiscectomy: Removing the herniated portion of the disc.
- Laminectomy: Removing part of the vertebra to relieve pressure on the nerves.
- Spinal Fusion: Stabilizing the spine in severe cases of instability.
Preventing Disc Herniation
Prevention is always better than cure. Here are some practical tips:
- Maintain Good Posture: Sit and stand with your back straight.
- Exercise Regularly: Focus on strengthening your core muscles.
- Lift Properly: Bend your knees and keep your back straight when lifting heavy objects.
- Stay Active: Avoid prolonged sitting or standing.
- Watch Your Weight: Excess weight puts extra strain on the spine.
Why This Information Matters
Disc herniation can significantly impact your quality of life if not managed properly. By understanding the four types of herniation and their symptoms, you can take proactive steps to prevent, diagnose, and treat the condition effectively.
FAQs
What are the 4 stage of disc herniation?
The four stages of disc herniation are:
- Degeneration ,
- Prolapse (or Bulging),
- Extrusion,
- Sequestration
What are the four grades of disc herniation?
The grades are used to describe the severity of disc herniation:
Grade 1: Mild bulging or slight deformation.
Grade 2: Moderate bulging with some pressure on nerves.
Grade 3: Significant extrusion, with noticeable pressure on the spinal nerves.
Grade 4: Severe sequestration, where parts of the disc break off and move around, causing major nerve damage.
How many types of herniated discs are there?
There are four main types of herniated discs: bulging, protrusion, extrusion, and sequestration. These types are based on how much the disc has moved or broken.
Where are the types of disc herniation?
The types of disc herniation usually occur in the spine, specifically in the neck (cervical), mid-back (thoracic), or lower back (lumbar). The most common location is the lower back.