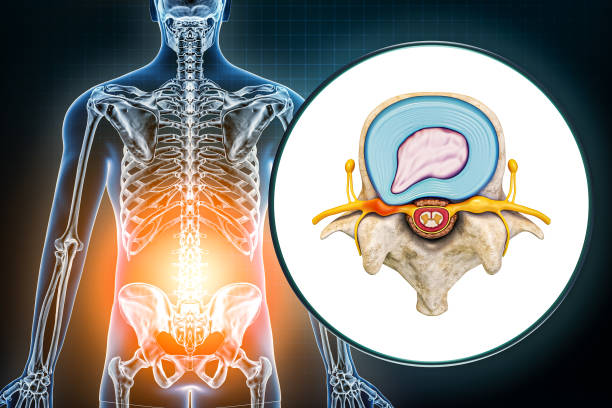
A medical condition affecting the lumbar spine, PLID (Prolapsed Lumbar Intervertebral Disc) occurs when a tear in the outer fibrous ring (annulus fibrosus) of an intervertebral disc allows the soft, central portion (nucleus pulposus) to bulge out beyond the damaged outer ring. This tear can release inflammatory chemical mediators, leading to severe pain, even without nerve root compression. Understanding PLID is crucial for effective treatment and management strategies.
Types Of Herniation:
- Posterolateral disc herniation
- Central herniation
- Lateral disc herniation
Posterolateral disc Herniation:
The protrusion is usually posterolateral into the vertebral canal and compresses the roots of the spinal cord. The protruded disc usually compresses the next lower nerve as that nerve crosses the level of the disc in its path to its foramen, e.g. protrusion of the 5th lumbar disc usually affects S1 instead.
Central Herniation:
Less frequently, a protruded disc above the 2nd lumbar vertebra may compress the spinal cord itself or may result in cauda equina syndrome. In the lower lumbar segments, central herniation may result in S1 radiculopathy.
Lateral Disc Herniation:
May compress the nerve root above the level of the herniation. L4 nerve root is most often involved & patients typically have intense radicular pain.
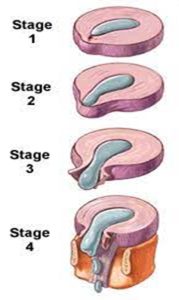
Stages of Disc Herniation:
Stage 1: Disc Compression.
Stage 2: Bulging Disc.
Stage 3: Disc Protrusion.
Stage 4: Herniated Disc
Epidemiology:
Disc herniation can occur in any disc. The two most common forms are lumbar and cervical disc herniation. The former is the most common causing lower back pain (lumbago) and often leg pain as well (sciatica). Lumbar disc herniation occurs 15 times more often than cervical disc herniation. Most disc herniations occur in the thirties or forties when the nucleus pulposus is still a gelatin-like substance. With age the nucleus pulposus changes (dries out) and the risk of herniation is greatly reduced. Mostly at the L4/5 level.
Causes of PLID:
- Unaccustomed work
- Bad posture
- Overweight
- Heavy weight lifting
- Prolong standing/ sitting
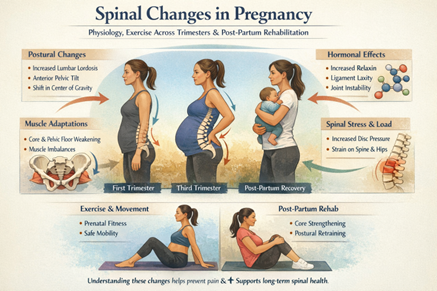
- Pregnancy
- Strenuous activity
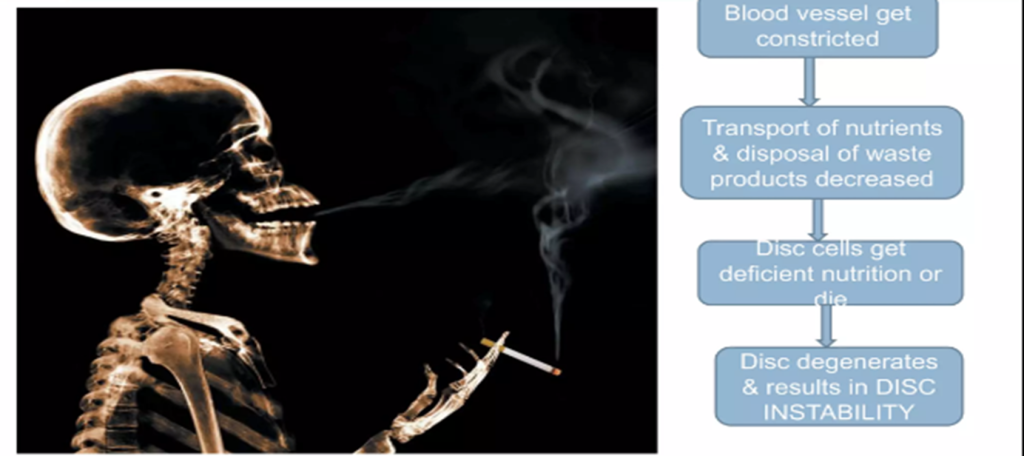
Effect of smoking:
History:
- Age: 20-45yrs
- Pain starts while lifting/ forward bending.
- Radiation: Towards buttock, lower limbs.
- It is worsened by coughing or straining.
- Later paraesthesia /numbness in legs/ feet.
- Cauda equina: urinary retention & perineal numbness.
- Muscle Weakness
Clinical Features:
- Vary depending on the location of the herniation and the types of soft tissue that become involved.
- Often herniated discs are not diagnosed immediately, as the patients come with undefined pains in the thighs, knees, or feet.
- Unlike pulsating pain by muscle spasm, pain from a herniated disc is usually continuous or at least is continuous in a specific position of the body.
- If the disc protrudes to one side, it may irritate the dural covering of the adjacent nerve root causing pain in the buttock, posterior thigh, and calf ( sciatica).
- Neurological changes such as numbness, tingling, muscular weakness, paralysis, paresthesia, and affection of reflexes.
- A large central rupture may cause compression of the cauda equina.
- Sometimes a local inflammatory response with edema aggravates the symptoms.
Features of Cauda Equina Syndrome:
- Bladder and bowel incontinence.
- Perineal numbness.
- Bilateral sciatica.
- Lower limb weakness.
- Crossed straight leg raising sign.
Physical Examination:
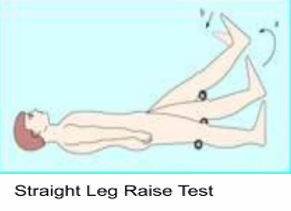
The straight leg raise test is positive if the pain in the sciatic distribution is reproduced between 30* and 70* passive flexion of the straight leg. Dorsiflexion of the foot exacerbates the pain.
Root Tension Signs:
Straight leg raising: L5, S1 root.
Contralateral SLR: Sequestrated or extruded disc.
Femoral Stretching, reverse SLR: L3, L4 root.
Diagnosis:
Examination in a patient with suspected lumbar ( intervertebral ) disk disease may feature the following:
- Abnormal Gait
- Abnormal postures
- Decreased lumbar range of motion
- Positive straight leg raising test: Indicative of nerve root involvement.
Differential Diagnosis of Plid:
- Mechanical Pain
- Discogenic Pain
- Spondylosis/Spondylolisthesis
- Spinal Stenosis
- Hematoma
- Discitis
- Mass Lesion/ Malignancy
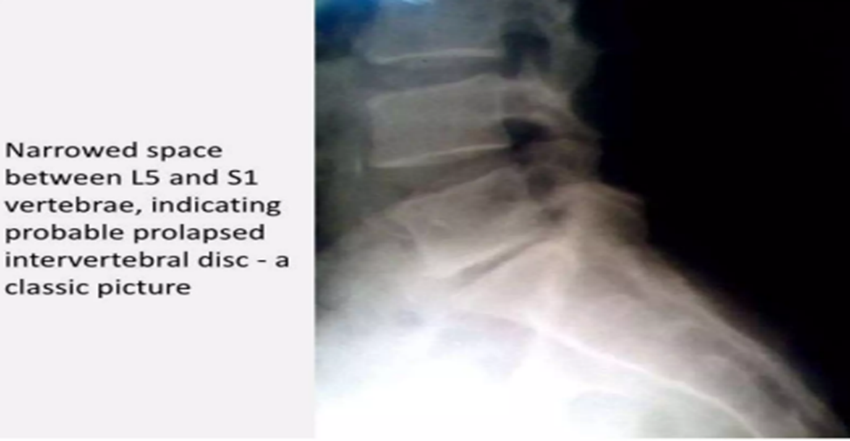
Investigations:
- X-rays: lumbosacral spine
Loss of lumbar lordosis
Narrowed disc spaces
- CT scan: lumbar spine
Shape and size of the spinal canal and its contents and structures around it.
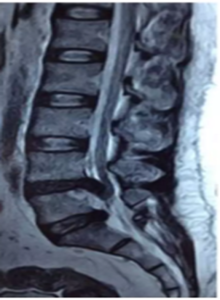
- MRI: lumbar spine
Intervertebral disc protrusion
Bulging out disc
Compression or nerve root
Physical Therapy Protocol:
Conservative Management:-
► Aim of physiotherapy
- Accelerate healing.
- To relieve pain.
- To restore mobility.
- To restore posture & strength
- Prevention
► To accelerate healing:-
- Rest:-1-2 days but in severe cases 7 to 10 days (1 to 2wks.)
- Corset or lumber belt (L-S belt).
- If severe disabling pain crutches are advised
- Elastic adhesive strapping is applied over the back to immobilize the spine. It should be used up to 10 days & replace the tape 2 to 3 times.
► To relieve pain:-
Traction:- ICT & ILT are used to relieve intradiscal pressure & increase the disc space.
► Electrotherapy modalities:
Cryotherapy: reduces muscle spasms and inflammation in acute phase.
TENS: relieves pain in both acute and chronic phases.
UST: as phonophoresis increases the extensibility of connective tissues
Moist heat: used as an adjunct before applying specialized techniques to decrease muscle spasms.
SWD-pulsed: SWD in acute conditions and continuous SWD in chronic cases for 20 to 25 minutes.
LWD pulsed SWD in acute conditions and continuous SWD in chronic cases. 08 to 12 minutes.
IFT – 20 to 25 mints
LASER:- Laser therapy treatment is a very advanced method for pain relief and decreased inflammation.
► To restore mobility.
- Mobility exe.:- Mobility exe. of SI & hip can also include.
- AROM exercises within pain-free range to the lower limb can be done e.g.- ankle toe movements, heel drag, hip abduction/adduction.
- Mobilization of thoracic spine mobilization of segments above and below the affected segmental level.
- Piriformis/ Hams/ Calf muscle stretching
- Maintain/ improve mobility of neural tissues- SLR with foot dorsiflexion.
► To restore posture & strength
- Spinal extension/ strengthening exe:- In initial stage movt. of the spine is contraindicated but after the subside of pain, the isometric spinal exe & then the isotonic spinal exe.
- Local support in the form of the corset (lumbosacral belt), abdominal binder, tape, etc.
► Prevention:
Posture and activity modification- Avoid forward bending, sitting for a long duration, or lifting activities.
LUMBAR STABILISATION PROGRAMME
A) Soft tissue flexibility:-
1) Hamstring m/s tendinous unit stretching
2) Quads m/s tendinous unit stretching
3) Iliopsoas m/s tendinous unit stretching
4) Gastrosoleus m/s tendinous unit stretching
5) External and internal hip rotators.
B) Stabilisation Programme:-
1) Prone Gluteal squeeze with arm raise with alternate arm raise with leg raise with alternate leg raise alternate arm & leg raises
2) Supine pelvic bracing
3) Bridging programme
- Basic Position
- One leg raised with ankle wt.
- Stepping
- Balancing with Gymball
4) Quadruped with alternate one-arm & leg movement
5) Kneeling stabilisation.
6) Wall slide quadriceps strengthening
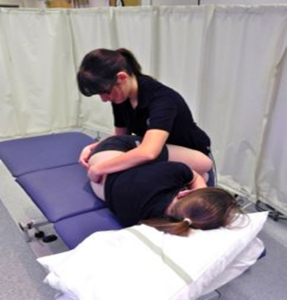
Passive Intervertebral Movement Mobilization Technique:
- The patient lies on their side with hips and knees flexed. The therapists position themselves in front of the patient.
- The therapist reaches under the patient’s knees, lifting them up and resting the patient’s lower legs against the therapist.
- The therapist places their fingers on the spinous process of the segment to be assessed for movement
- To produce passive flexion the therapist rocks from side to side with their pelvis, carrying the patient’s legs along with them.
- Opening and closing of the interspinous gaps can be felt as the patient is passively flexed.
Mobilization with Movement:
- The patient is standing perpendicular to the therapist.
- Therapists need to stabilize the pelvis by placing the cup of hand over the ASIS.
- The therapist palpates between adjacent spinous processes.
- The patient actively flexes the lumbar spine and then extends to return to the neutral position.
- The problematic level is palpated and when the patient actively moves into flexion, a sustained PA force is applied to the spinous process throughout the movement.
About Authors
Dr. Muhammad Mahmood Ahmad is a Spinal as well as an Orthopedic Surgeon with over 14 years of experience currently practicing at Razia Saeed Hospital, Multan.