Disc herniation is a common spinal condition that affects millions, often resulting in pain, discomfort, and reduced mobility. By understanding the 4 stages of disc herniation, individuals can better identify symptoms, seek appropriate treatment, and take proactive steps toward recovery. This guide provides a clear and authoritative explanation of disc herniation, from its early stages to advanced treatments, empowering readers to make informed decisions.
The 4 Stages of Disc Herniation Explained (MRI Insights)
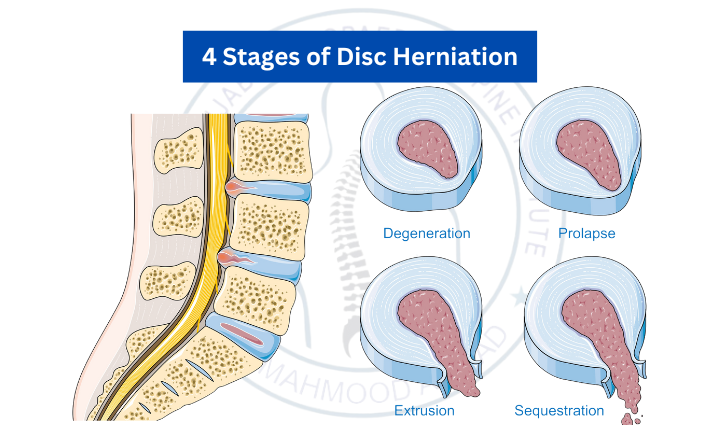
Disc herniation progresses through distinct stages, each marked by changes visible on MRI scans. Let’s examine these stages and their implications:
Stage 1: Disc Degeneration
In the earliest stage, wear and tear or aging cause the intervertebral discs to lose their flexibility and hydration. While the disc structure remains intact, its ability to cushion the spine diminishes.
MRI Findings: Thinning or slight bulging of the disc.
Symptoms: Minimal or no pain, mild stiffness, and occasional discomfort.
Treatment Focus: Preventing progression with physical activity, hydration, and spinal health practices.
Stage 2: Prolapse
As degeneration continues, the outer disc layer weakens, and the inner gel-like nucleus pulposus begins to push outward. This creates a noticeable bulge or protrusion in the disc.
MRI Findings: A bulging disc without rupture of the outer layer.
Symptoms: Back pain, localized discomfort, and occasional tingling if a nerve is compressed.
Treatment Focus: Non-invasive options like physical therapy, core-strengthening exercises, and anti-inflammatory medications.
Stage 3: Extrusion
At this stage, the nucleus pulposus breaks through the outer layer of the disc. This extrusion can put significant pressure on nearby nerves, leading to more severe symptoms.
MRI Findings: The inner disc material has pushed through the annulus fibrosus, but remains attached.
Symptoms: Radiating pain (e.g., sciatica), numbness, and muscle weakness.
Treatment Focus: Advanced treatments such as epidural steroid injections, specialized physical therapy, and surgical evaluation if symptoms persist.
Stage 4: Sequestration
In the final stage, fragments of the nucleus pulposus break free entirely and migrate into the spinal canal. This can lead to intense pain, severe nerve compression, and potential loss of function.
MRI Findings: Disc fragments detached from the main structure.
Symptoms: Severe pain, significant mobility issues, and neurological deficits such as bowel or bladder dysfunction.
Treatment Focus: Surgical interventions, including microdiscectomy or spinal fusion, are often required.
The Healing Process Stages of Recovery for a Herniated Disc
Recovery from disc herniation depends on its stage and the chosen treatment. Healing typically occurs in three overlapping phases:
Acute Phase (Weeks 1–6):
Focus: Pain relief and inflammation management.
Methods: NSAIDs, rest, and physical therapy to stabilize the spine.
Repair Phase (Months 1–3):
Focus: Tissue repair and nerve decompression.
Methods: Rehabilitation exercises and gradual return to daily activities.
Strengthening Phase (Months 3–6+):
Focus: Restoring mobility and preventing future injury.
Methods: Core strengthening, posture correction, and lifestyle adjustments.
The 4 Types of Disc Herniation
Disc herniation can manifest in different ways, each with unique challenges and treatments:
- Bulging Disc: The disc protrudes slightly, but the outer layer remains intact.
- Protrusion: The nucleus pulposus pushes against the annulus fibrosus, forming a noticeable bulge.
- Extrusion: The nucleus breaks through the annulus fibrosus but remains connected.
- Sequestration: Fragments of the nucleus break away and migrate into the spinal canal.
Understanding the type of herniation can guide more effective treatments.
Effective Lumbar Disc Herniation Treatment Protocols
The lumbar spine, or lower back, is the most common site for disc herniation. A structured treatment protocol can provide significant relief:
Phase 1: Immediate Relief
Rest, ice/heat therapy, and over-the-counter pain relievers like ibuprofen or naproxen.
Phase 2: Rehabilitation
Supervised physical therapy, core-strengthening exercises, and posture correction.
Phase 3: Interventional Treatments
Epidural steroid injections or nerve blocks for pain management.
Phase 4: Surgical Solutions
Options like microdiscectomy or artificial disc replacement for severe cases.
Recognizing Herniated Disc Symptoms by Stage
Each stage of disc herniation presents distinct symptoms, which can help in early diagnosis:
- Stage 1: Mild stiffness, occasional discomfort.
- Stage 2: Back pain, tingling, and minor nerve irritation.
- Stage 3: Radiating pain, numbness, and muscle weakness.
- Stage 4: Severe pain, mobility loss, and potential neurological issues.
Timely intervention can significantly improve outcomes, especially in the earlier stages.
Stage 4 Herniated Disc Treatment Options
Even in advanced cases, effective treatments can lead to recovery:
- Microdiscectomy: A minimally invasive surgery to remove the herniated portion of the disc.
- Spinal Fusion: Stabilizes the affected area for improved function and reduced pain.
- Artificial Disc Replacement: Preserves mobility by replacing the damaged disc with a synthetic one.
These treatments are often combined with post-surgical physical therapy to ensure optimal recovery.
Non-Surgical Disc Protrusion Treatment
Non-surgical treatments are often sufficient for early-stage herniation:
- Physical Therapy: Tailored exercises improve spinal stability and flexibility.
- Traction Therapy: Reduces disc pressure through controlled spinal stretching.
- Chiropractic Care: Realigns the spine to relieve tension and nerve compression.
- Lifestyle Adjustments: Regular exercise, ergonomic workspaces, and a healthy diet support long-term spinal health.
Best Painkillers for Herniated Discs
Pain management is crucial during recovery. The best medication depends on the severity of symptoms:
- Mild Pain: NSAIDs like ibuprofen or acetaminophen.
- Moderate Pain: Prescription-strength NSAIDs or corticosteroid injections.
- Severe Pain: Nerve pain medications (e.g., gabapentin) or short-term opioids under medical supervision.
Always consult a healthcare provider to ensure safe and effective use of medication.
Frequently Asked Questions (FAQs)
Can a herniated disc heal naturally?
Yes, many mild cases improve with rest, physical therapy, and proper care.
How long does it take to recover from a herniated disc?
Recovery varies, typically ranging from a few weeks to several months depending on the severity and treatment.
What are the red flags of advanced herniation?
Severe pain, loss of mobility, or bowel/bladder dysfunction require immediate medical attention.
Is surgery always necessary?
No, most cases are treated conservatively, but surgery may be needed for severe or persistent symptoms.
What lifestyle changes help prevent recurrence?
Maintaining a healthy weight, exercising regularly, and practicing good posture reduce the risk of future herniation.
What are PLID stages, and how do they relate to disc herniation?
PLID stages refer to the progressive phases of posterior longitudinal interligament disc issues, similar to the stages of disc herniation described in this article.
Final Thoughts
The 4 stages of disc herniation may sound daunting, but advancements in diagnosis and treatment have made recovery more achievable than ever. By understanding the stages, symptoms, and available treatments, you can take control of your spinal health and regain your quality of life. Seek professional guidance, stay proactive, and embrace a healthier future because a pain-free life is within reach!